Vitamin D and Bone Health: What Really Works for Strong Bones
For decades, doctors told us: take vitamin D to protect your bones. It’s simple, logical, and easy to believe. But what if the advice you’ve been following is outdated-or even harmful? The truth about vitamin D and bone health isn’t what you think. It’s not about popping a high-dose pill every day. It’s not about chasing the highest number on a blood test. And it’s not one-size-fits-all.
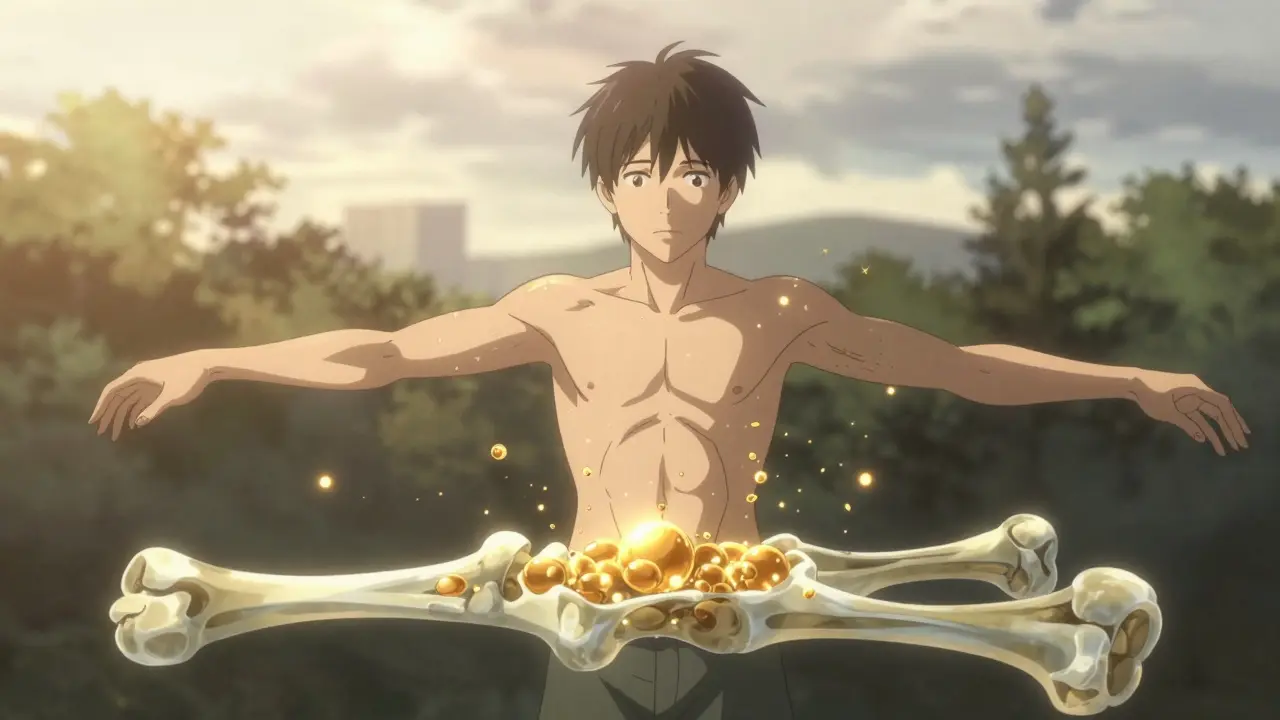
Why Vitamin D Matters for Your Bones
Vitamin D isn’t just a supplement. It’s a hormone your body makes when your skin touches sunlight. Its main job? Help your gut absorb calcium. Without enough vitamin D, your body absorbs only 10-15% of the calcium you eat. With enough, that jumps to 60-80%. That’s the difference between weak, porous bones and strong, dense ones.
It’s not just about calcium, though. Vitamin D also helps your bones renew themselves properly. Old bone breaks down, new bone forms. Vitamin D keeps that cycle balanced. And it strengthens your muscles. Stronger muscles mean fewer falls-and fewer broken hips, especially as you get older.
This isn’t theory. It’s been known since the 1920s, when researchers found vitamin D cured rickets, a disease that warped children’s bones. But today, we’re learning the hard way: more isn’t always better.
What’s the Right Level of Vitamin D?
For years, the standard was clear: your blood level of 25-hydroxyvitamin D (25(OH)D) should be at least 30 ng/mL. That’s what the Endocrine Society said. That’s what many doctors still recommend.
But then came the VITAL trial-a massive, 5-year study led by Harvard Medical School. It followed over 25,000 healthy adults, half taking 2,000 IU of vitamin D daily, half taking a placebo. After five years, there was no difference in fracture rates. Not in hips. Not in wrists. Not in spine.
Even more surprising? People with levels below 20 ng/mL (deficient) didn’t get fewer fractures by taking extra vitamin D. And people with levels above 30 ng/mL didn’t get stronger bones from higher doses.
So what’s the real target? For most healthy adults, 20 ng/mL is enough. That’s the level the Institute of Medicine stands by. Anything above that? It doesn’t seem to add protection for bones.
The Dangerous Myth of High-Dose Supplementation
Here’s where things get risky. Many people take 5,000 IU, 10,000 IU, even more-thinking they’re doing their bones a favor. But a 2020 JAMA study showed something shocking: high doses actually lowered bone density.
Participants who took 4,000 IU daily lost 3.9 mg of bone mineral per cm³ in their radius (forearm bone). Those on 10,000 IU lost 7.5 mg. That’s not a fluke. That’s a direct effect. Higher doses didn’t make bones stronger. They made them weaker.
Why? One theory: too much vitamin D overstimulates bone turnover. Your body breaks down bone faster than it rebuilds it. Another: excess vitamin D may interfere with other minerals like magnesium and phosphorus, which also play roles in bone health.
And it’s not just bone density. High doses can raise calcium levels in your blood. That can lead to kidney stones, calcified arteries, or even heart rhythm problems. The body isn’t designed to handle mega-doses of vitamin D. It’s designed for steady, moderate levels.
Who Actually Needs Supplements?
If most healthy people don’t benefit from extra vitamin D, who does?
- People with documented deficiency (below 20 ng/mL): These are the ones who need it most. A short course of 1,000-2,000 IU daily for 3-6 months can fix it.
- Older adults with limited sun exposure: If you’re indoors most of the day, live in a northern climate, or wear sunscreen all the time, your skin isn’t making enough.
- People with obesity: Fat cells trap vitamin D. Someone with a BMI over 30 may need double the dose to reach the same blood level as someone with normal weight.
- Those with malabsorption conditions: Crohn’s disease, celiac disease, gastric bypass surgery-all can block vitamin D absorption.
For everyone else? Focus on food and sun. A 3-ounce serving of salmon gives you 570 IU. Fortified milk? 100 IU per cup. Egg yolks? 44 IU each. You’d need to eat 10 eggs and drink 5 glasses of milk daily to hit 1,000 IU-hard to do without supplements.
But you don’t need to. If you get 10-15 minutes of midday sun on your arms and face, 2-3 times a week, your body makes plenty. No pills needed.
Calcium and Vitamin D Together: The Real Key
Here’s the missing piece: vitamin D alone doesn’t build bone. Calcium does. And the two work best together.
A 2023 meta-analysis found that when people took calcium and vitamin D together, hip fracture risk dropped by 30%. But here’s the twist: the benefit only happened with vitamin D doses under 400 IU per day. Higher doses? No effect.
That means: if you’re taking vitamin D to protect your bones, don’t go overboard. Keep it at 600-800 IU daily, and make sure you’re getting 1,000-1,200 mg of calcium from food or supplements.
Good sources of calcium? Dairy (milk, yogurt, cheese), leafy greens (kale, bok choy), canned salmon with bones, fortified plant milks, and tofu made with calcium sulfate.
Don’t rely on supplements alone. Food gives you other nutrients-magnesium, vitamin K, zinc-that also support bone health. Pills can’t replicate that.

Choosing a Supplement: What to Look For
If you need a supplement, here’s how to pick one that works:
- Choose D3, not D2. D3 (cholecalciferol) is the form your body makes from sunlight. It’s 87% more effective at raising blood levels than D2 (ergocalciferol), which comes from plants.
- Take it with your biggest meal. Vitamin D is fat-soluble. Taking it with dinner-especially if it has some fat-boosts absorption by up to 57%.
- Look for third-party tested brands. ConsumerLab’s 2022 review found 15% of vitamin D supplements had less than 90% of the labeled dose. One brand had only 72%. Others had over 120%. Stick to trusted brands like Thorne, Nordic Naturals, or Garden of Life.
- Avoid mega-doses. No need for 5,000 IU or 10,000 IU unless you’re under a doctor’s care for confirmed deficiency.
And don’t forget: timing matters. Check your blood level 3 months after starting or changing your dose. That’s how long it takes to reach steady state. Don’t test after 2 weeks. It won’t tell you anything real.
What’s Changing in 2026?
Guidelines are shifting fast. The U.S. Preventive Services Task Force still says: don’t take vitamin D to prevent fractures in healthy adults. The American Geriatrics Society reports a 22% drop in high-dose prescriptions since 2020. More doctors are starting to ask: “Do you even need this?”
Meanwhile, new research is pointing toward personalization. Your genetics, your weight, your skin tone, your location-all affect how much vitamin D you need. The D-Health Trial in Australia, finishing in 2024, is testing monthly 60,000 IU doses in 21,000 people over 60. That could change how we think about dosing.
And there’s a new drug on the horizon: eldecalcitol. It’s a synthetic vitamin D analog approved in Japan for osteoporosis. It cuts vertebral fractures by 37% compared to regular vitamin D. But it’s not available in the U.S. or Australia yet. And it’s not for prevention-it’s for treatment.
For now, the message is clear: stop chasing high numbers. Stop taking mega-doses. Focus on what works: moderate sun, decent diet, and just enough supplement if you truly need it.
What to Do Now
Here’s your simple plan:
- If you’re healthy, active, and get regular sun, you probably don’t need a supplement.
- If you’re over 60, indoors most days, or have dark skin, take 600-800 IU of D3 daily.
- Make sure you’re getting 1,000-1,200 mg of calcium from food.
- If you’re unsure, get a blood test for 25(OH)D. Don’t guess.
- If your level is below 20 ng/mL, work with your doctor. A short course of 1,000-2,000 IU daily for 3-6 months is usually enough.
- Avoid anything over 4,000 IU daily unless you’re under medical supervision.
Bone health isn’t about pills. It’s about balance. Your body knows what to do. You just need to give it the right tools-and not overload it with too much of a good thing.





Comments
sam abas
January 14, 2026 AT 19:30so i read this whole thing and honestly? i think the real problem is we’ve been brainwashed by supplement companies and doctors who get kickbacks from pharma. vitamin d isn’t a magic bullet, and yeah, i’ve seen people on 10k iu for years and their bones are still crumbling. but here’s the kicker-nobody talks about how much magnesium they’re also taking. if you’re not getting enough mg, all that vitamin d just sits there like a useless ornament. i’ve been taking 600 iu d3 + 400mg mg for 2 years now, and my bone density scan actually improved. no pills, no drama. just basics.
John Pope
January 16, 2026 AT 16:21ah yes, the myth of ‘moderation’-a doctrine crafted by the pharmaceutical-industrial complex to keep us docile while they monetize osteoporosis. we’ve been conditioned to believe that biology is a dial you can turn, not a symphony you conduct. vitamin d isn’t a nutrient-it’s a *signal*. and when you flood the system with synthetic analogs, you’re not just disrupting calcium homeostasis-you’re silencing the epigenetic whisper of ancestral sun exposure. the body doesn’t want pills. it wants dawn. it wants skin on stone. it wants the slow, sacred rhythm of daylight. and yet we swallow capsules like sacraments, blind to the fact that we’ve turned evolution into a pharmacy receipt.
Clay .Haeber
January 16, 2026 AT 17:24oh wow. someone actually read the entire VITAL trial summary and didn’t just scream ‘more d3!’ like a cult member at a wellness retreat. how refreshing. i’m so tired of people treating vitamin d like it’s the holy grail of health. it’s not. it’s a hormone. and if you’re taking 5k iu because your influencer said so, you’re basically doing the same thing as those people who chug celery juice to cure their anxiety. congrats-you’re not broken, you’re just over-supplemented.
Priyanka Kumari
January 17, 2026 AT 12:42This is such a balanced and important perspective. I’ve worked with elderly patients who were on high-dose vitamin D for years, and many had no improvement in bone density-some even had elevated calcium levels. The key takeaway? It’s not about the number on the bottle, it’s about the context: diet, sun, movement, and magnesium. I always tell my clients: food first, supplement only if needed, and always test before you mega-dose. Thank you for sharing evidence over hype.
Nelly Oruko
January 18, 2026 AT 15:22you don’t need a pill.
Scottie Baker
January 20, 2026 AT 00:07oh so now we’re supposed to believe the government and big pharma when they say ‘less is more’? right. because they’ve never lied before. you think they don’t profit off people being osteoporotic? they make billions on bisphosphonates and bone scans. you’re just another sheep swallowing the ‘safe dose’ narrative because it’s convenient. if you’re not taking at least 5k iu, you’re basically letting your bones rot. i’ve seen it. i’ve lived it. and i’m not backing down.
Rosalee Vanness
January 20, 2026 AT 06:20reading this made me feel so much less guilty about not taking supplements. i’ve been avoiding them for years because i just didn’t feel right about it-like i was forcing my body to do something it wasn’t meant to. but i never had the science to back it up. now i know: if i’m eating salmon twice a week, getting sunlight on my face during lunch, and drinking fortified oat milk, i’m probably fine. and honestly? that’s way less stressful than chasing a blood number. thank you for giving me permission to just… be. no pills, no guilt.
Trevor Davis
January 21, 2026 AT 12:05Interesting. I’ve been on 2000 IU daily for 3 years since my doctor said I was deficient. My level is now 48 ng/mL. Should I cut back? Or is this still safe? I’ve read conflicting things. Also-do you think D3 with K2 helps? I’ve started taking that combo.
John Tran
January 22, 2026 AT 10:52ok so i just wanna say… i think the real villain here is not vitamin d… it’s the *idea* of control. we live in a world where we think we can fix everything with a pill. but bones? they’re not a battery you charge. they’re a living ecosystem. you can’t out-supplement a sedentary life. you can’t out-pill a lack of gravity. you can’t out-d3 a life spent indoors. the real tragedy isn’t low vitamin d-it’s that we’ve forgotten how to *live*. walk outside. lift heavy things. eat real food. stop treating your body like a broken machine that needs a firmware update.
mike swinchoski
January 23, 2026 AT 09:33you’re all wrong. vitamin d is a scam. it’s all about calcium. if you don’t eat dairy, you’re doomed. period. i’ve been taking 2000mg of calcium daily since i was 30 and my bones are like steel. no sun, no d3, just milk, cheese, and yogurt. if you’re not eating dairy, you’re just fooling yourself. science says dairy = strong bones. end of story.
Trevor Whipple
January 23, 2026 AT 15:17lol at all these people acting like they’re the first to discover that more isn’t better. i’ve been saying this since 2018. the real issue? people take d3 and think they’re immune to osteoporosis. nope. you still need weight-bearing exercise. you still need protein. you still need to not smoke. you still need to not be 90 and sitting on a couch all day. vitamin d is a tiny piece of a giant puzzle. stop treating it like the whole damn jigsaw.