Timing Medication Doses: How Administration Time Affects Side Effects
Medication Timing Window Calculator
How Strict Is Your Medication's Timing?
Find your safe timing window based on medication criticality
Why Timing Matters
Your body's circadian rhythm affects how medications work. Taking a drug at the wrong time can:
- Reduce effectiveness by 15-20%
- Double bleeding risk for blood thinners
- Trigger hypoglycemia with insulin
- Compromise cancer treatment
Ever wonder why your doctor told you to take your blood pressure pill at night, or your statin right before bed? It’s not just a random suggestion. The time you take your medication can make a real difference-sometimes even more than the dose itself. Taking a drug at the wrong time doesn’t just reduce its effectiveness; it can turn a safe treatment into a risky one. For some medications, a 30-minute delay can mean the difference between feeling fine and ending up in the hospital. This isn’t guesswork. It’s science.
Why Timing Matters More Than You Think
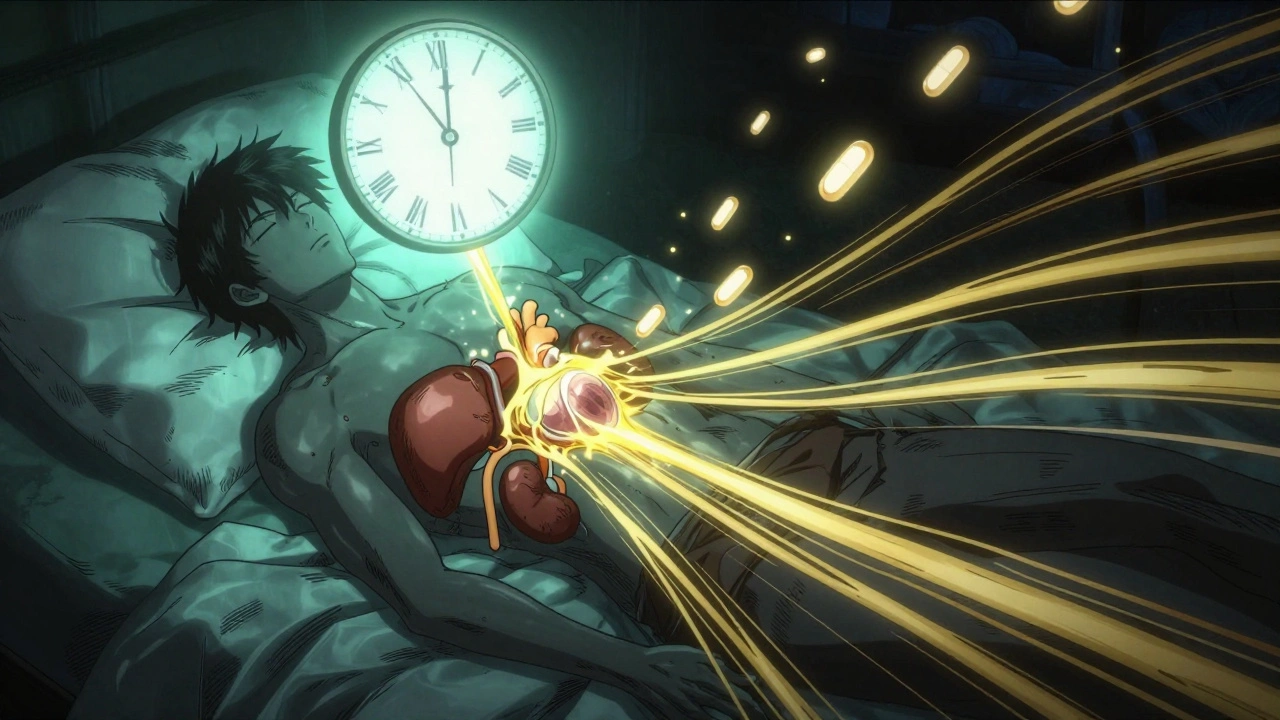
Your body runs on a 24-hour clock. Not just your sleep cycle-your liver, kidneys, heart, and even your stomach lining follow a rhythm. These daily cycles control how your body absorbs, breaks down, and gets rid of drugs. When you take a medication, you’re not just giving it to your body-you’re asking it to interact with a system that’s constantly changing. Take statins, for example. These cholesterol-lowering pills work best when taken at night. Why? Because your liver makes most of its cholesterol while you’re asleep. If you take the pill in the morning, you’re missing the peak window. Studies show evening dosing can lower LDL (bad) cholesterol by 15-20% more than morning doses. That’s not a small gain-it’s the difference between needing a second drug or avoiding it altogether. Same goes for blood pressure meds. ACE inhibitors like lisinopril or losartan are more effective-and safer-when taken at bedtime. The MAPEC study found that patients who took their blood pressure pills at night had a 29% lower risk of heart attack, stroke, or heart failure over five years. Why? Because nighttime dosing better controls the early morning blood pressure spike, which is when most cardiovascular events happen.High-Risk Medications: When Timing Can Be Life or Death
Not all meds are created equal when it comes to timing. Some can tolerate being taken an hour late. Others? Not even 15 minutes. Insulin is one of the most timing-sensitive drugs out there. If you take rapid-acting insulin too early before a meal, your blood sugar can crash. Too late, and your sugar spikes dangerously high. Mistimed insulin causes hypoglycemia in about 22% of cases, according to clinical data. That’s not just uncomfortable-it’s dangerous. Falls, seizures, even coma can follow. Anticoagulants like warfarin or apixaban are another big one. These thin your blood to prevent clots, but they’re a tightrope walk. If you take them at inconsistent times, your INR levels (a measure of blood clotting) swing wildly. Timing errors can increase bleeding risk by up to 37%. That’s why many clinics now require patients to take these meds at the exact same time every day-no exceptions. Chemotherapy drugs? Timing matters there too. Deviating more than 30 minutes from the scheduled time can reduce effectiveness by 15-20%. Why? Because cancer cells go through phases of growth, and some chemo drugs only work when cells are dividing. If you miss the window, you’re not killing as many cells-and the cancer gets a chance to bounce back.What About the Other Drugs? Not All Timing Is Critical
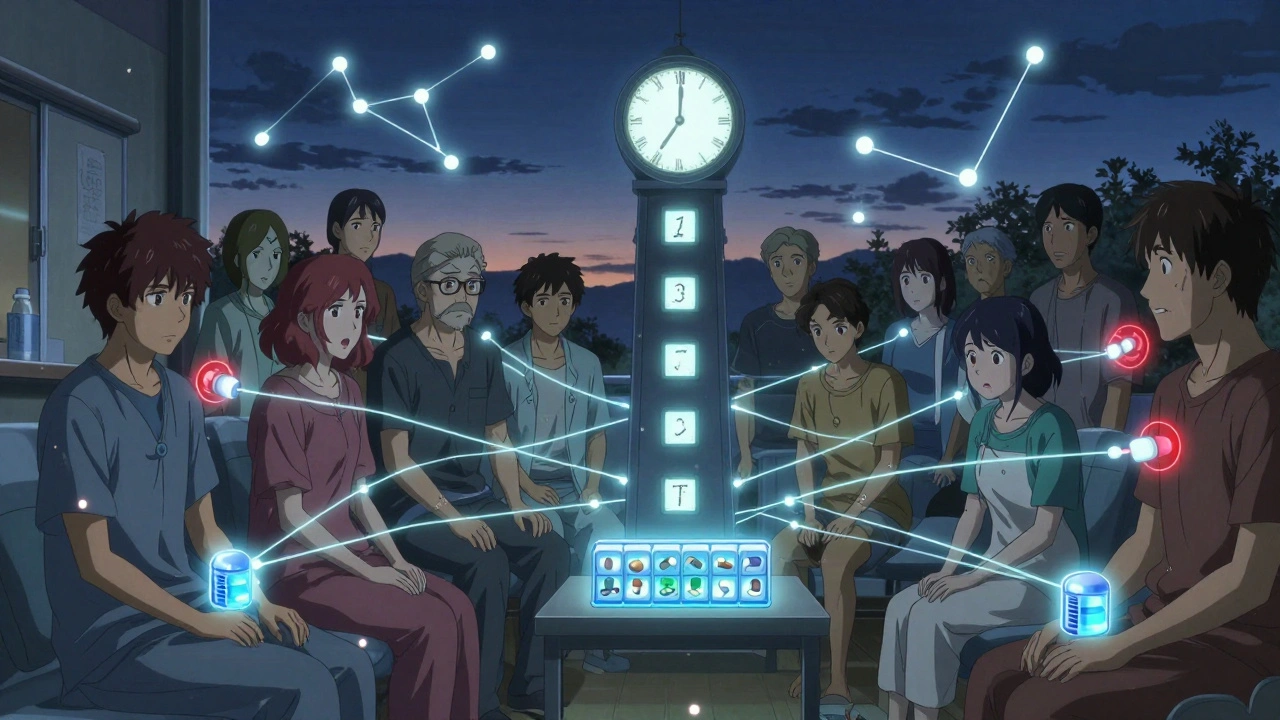
You don’t need a stopwatch for every pill. Many medications are forgiving. Take hydrochlorothiazide, a common water pill for high blood pressure. A 12-hour delay? Probably no big deal. Your body handles it fine. Same with antibiotics like amoxicillin. While it’s ideal to space them evenly (every 8 or 12 hours), studies show that taking them 2-3 hours off schedule rarely affects outcomes. The goal here is consistency, not precision. The key is knowing which category your drug falls into. Medications can be grouped by timing criticality:- High criticality: Insulin, anticoagulants, chemotherapy, morphine (for cancer pain), some anti-seizure drugs. Window: ±15-30 minutes.
- Moderate criticality: Statins, ACE inhibitors, beta-blockers, thyroid meds. Window: ±1-2 hours.
- Low criticality: Most antibiotics, pain relievers like ibuprofen, most vitamins. Window: ±4-6 hours or more.

Why Do People Keep Getting It Wrong?
If this is so important, why are so many people still taking meds at the wrong time? The answer? Life gets messy. Nurses in hospitals get interrupted up to five times during a med pass. Studies show each interruption increases the chance of a timing error-from 39% to 61%. At home, it’s worse. A survey of 1,200 patients found 68% missed their scheduled time for chronotherapeutic meds. Why? Work schedules, forgetfulness, sleep disruptions, or just not knowing it mattered. Health literacy plays a huge role. People with low health literacy-74% of those who miss doses-don’t understand why timing matters. They think, “It’s just a pill. As long as I take it, it’ll work.” That’s not true. For some drugs, it’s like turning on a light switch at the wrong hour-it just doesn’t do what it’s supposed to.How to Get It Right
You don’t need to be a nurse to get your timing right. Here’s how to make it simple:- Ask your doctor or pharmacist: “Is the timing of this pill important?” Don’t assume. If they say yes, ask what window is acceptable.
- Use a pill organizer with alarms: Simple phone alarms or smart pill dispensers (like MedMinder) can remind you at the exact time. Set two: one 15 minutes before, one at the time.
- Link it to a habit: Take your statin with your nighttime toothbrushing. Take your blood pressure pill with your morning coffee. Anchor it to something you already do.
- Keep a log: Jot down when you took each dose for a week. You’ll spot patterns. Did you skip your evening pill because you were out to dinner? Adjust the schedule if your doctor says it’s safe.
- Check your meds regularly: Every few months, review your list with your pharmacist. New meds? Changed doses? Timing rules might’ve changed too.
What’s Changing in Healthcare
Hospitals and clinics are catching on. The FDA now asks drug makers to include circadian rhythm data in new drug applications-up from just 3 in 2018 to 17 in 2022. Electronic health records like Epic now have built-in tools (ChronoCare module) that flag when a patient’s timing is off for high-risk drugs. Academic hospitals are leading the way. 42% have formal chronotherapy protocols. Community hospitals? Only 14%. But that gap is closing. The American College of Clinical Pharmacy officially endorsed chronotherapy in 2022. That’s a big deal-it means this isn’t a fringe idea anymore. It’s standard practice. The global market for chronotherapy tools is expected to hit $32.4 billion by 2027. Why? Because it works. And it’s cheap. No new drugs. No higher doses. Just better timing. That’s the beauty of it.The Bottom Line
Timing isn’t just a detail. For some medications, it’s the most important part of your treatment. A missed hour can mean more side effects, less protection, or even a trip to the ER. But it’s not about perfection. It’s about awareness. If you’re on insulin, blood thinners, or chemo-be strict. Use alarms. Stick to the window. If you’re on a statin or a blood pressure pill-try to be consistent, especially at night. For most others? Don’t stress. Just take it when you can. The science is clear: your body has a rhythm. Medications work best when they sync with it. You don’t need to be a scientist to use this knowledge. You just need to ask the right questions-and then act on the answer.Does the time I take my medication really affect side effects?
Yes, for many medications. Your body’s circadian rhythm affects how drugs are absorbed, metabolized, and cleared. Taking a drug at the wrong time can increase side effects like low blood sugar (with insulin), bleeding (with blood thinners), or muscle pain (with statins). For some, timing can be just as important as the dose itself.
Which medications are most sensitive to timing?
High-risk medications include insulin, anticoagulants (like warfarin or apixaban), chemotherapy drugs, and certain pain medications like morphine. These often require administration within a 15-30 minute window. Statins and blood pressure medications like ACE inhibitors also benefit from consistent timing-especially evening doses-for maximum benefit and fewer side effects.
Can I take my pills at a different time if it’s more convenient?
It depends. For statins, blood pressure meds, or antibiotics, shifting by 1-2 hours is usually fine. For insulin, blood thinners, or chemo, even a 30-minute delay can be risky. Always check with your doctor or pharmacist before changing your schedule. They can tell you what’s safe based on your specific meds.
Why do I need to take statins at night?
Your liver produces most of its cholesterol at night. Statins block an enzyme involved in that process. Taking them in the evening lines up the drug’s peak effect with your body’s peak cholesterol production-making them 15-20% more effective than morning doses.
How can I remember to take my meds at the right time?
Set phone alarms, use a pill organizer with built-in reminders, or link your dose to a daily habit like brushing your teeth or eating breakfast. For high-risk meds, consider a smart dispenser like MedMinder. Keeping a simple log for a week can also help you spot patterns and adjust your routine.



Comments
Doug Hawk
December 3, 2025 AT 06:04Had no idea statins worked better at night. My doc just said 'take it before bed' like it was a chore. Turns out my liver's doing a midnight shift and I'm just the delivery guy. Mind blown.
Also why the hell don't pharmacies print this on the label? I've lost count of how many times I took my BP med at 7am because that's when I woke up, not when it mattered.
Biggest takeaway: stop treating meds like candy. Timing's part of the dose.
John Morrow
December 4, 2025 AT 07:52The circadian pharmacokinetics of chronotherapeutic agents is a fascinating domain of pharmacodynamics, yet it remains woefully underutilized in clinical practice due to systemic inefficiencies in patient education and the structural inertia of primary care models. The MAPEC study, while methodologically robust, suffers from selection bias in its cohort, and the 29% relative risk reduction is contingent upon strict adherence to nocturnal dosing regimens-a luxury inaccessible to shift workers, the elderly, or those with comorbid cognitive impairment. Furthermore, the FDA’s recent push for circadian data inclusion in NDAs is more performative than substantive; the agency lacks enforcement mechanisms for temporal compliance in labeling. Until we integrate real-time pharmacokinetic monitoring via wearable biosensors into EHRs, this remains a theoretical framework masquerading as clinical protocol.
Kristen Yates
December 5, 2025 AT 20:55I’ve been taking my blood pressure pill at night for three years now. No more dizzy spells in the morning. I don’t know the science, but I know how I feel. Simple. Consistent. That’s all I need.
Saurabh Tiwari
December 5, 2025 AT 21:17bro this is wild 😮
took my warfarin at 8pm last night cause i saw this post
today i felt like a new man
also i got a pill box with alarms now 🙌
thanks for the info man
ps my grandma takes 7 pills and never knows when
gonna print this out for her
Michael Campbell
December 5, 2025 AT 23:53They want you to take pills at night so they can track you better. Big Pharma + EHR systems = surveillance. Wake up. They don’t care if you live. They care if you keep buying.
Victoria Graci
December 7, 2025 AT 03:13It’s like your body is a symphony and every drug is an instrument. Play the violin at the wrong tempo and the whole piece falls apart. We treat medicine like a vending machine-pop in the pill, get the result. But biology isn’t linear. It’s rhythmic. It breathes. It sleeps. It wakes. We’re not just dosing-we’re conducting. And if you don’t know the score, you’re just making noise.
That’s why insulin at 7am is a disaster. That’s why statins at noon are half as effective. We’ve forgotten that we’re not machines. We’re living cycles. And the best treatment isn’t stronger drugs-it’s syncing with the rhythm we were born with.
Carolyn Woodard
December 7, 2025 AT 20:10John Morrow’s comment above is technically accurate but misses the human reality. Most patients aren’t reading FDA guidelines-they’re juggling jobs, kids, and chronic pain. The real barrier isn’t ignorance-it’s access. Who has time to set 5 alarms? Who can afford MedMinder? The science is solid, but the delivery system is broken. We need low-tech, low-cost solutions baked into primary care-not more jargon for people who already feel like they’re failing.
Allan maniero
December 8, 2025 AT 14:44I’ve worked in a community pharmacy for 18 years and I can tell you-timing errors are the silent epidemic. We see it every day. A man takes his warfarin at 8pm one night, then 11am the next because he was out with his grandkids. No one tells him it matters. He doesn’t know to ask. We try to explain, but we’re rushed, understaffed, and the system doesn’t reward us for spending 10 minutes on a single patient. The fact that 68% of people miss their chronotherapeutic window? That’s not laziness. That’s a healthcare system that forgot to teach people how to survive their own treatment plan. We need pharmacists in every clinic, not just behind the counter.
Anthony Breakspear
December 9, 2025 AT 01:20Here’s the cheat code: link your pill to something you already do every day. Brush your teeth? Take your statin. Drink your coffee? Take your BP med. Make it part of the ritual, not a chore. I used to forget my thyroid med until I started taking it right after I poured my first cup. Now I don’t even think about it. It’s just part of my morning. No alarms. No apps. Just habit stacking. Try it. Your future self will thank you.
Also-yes, your liver is a night owl. Respect it.
Zoe Bray
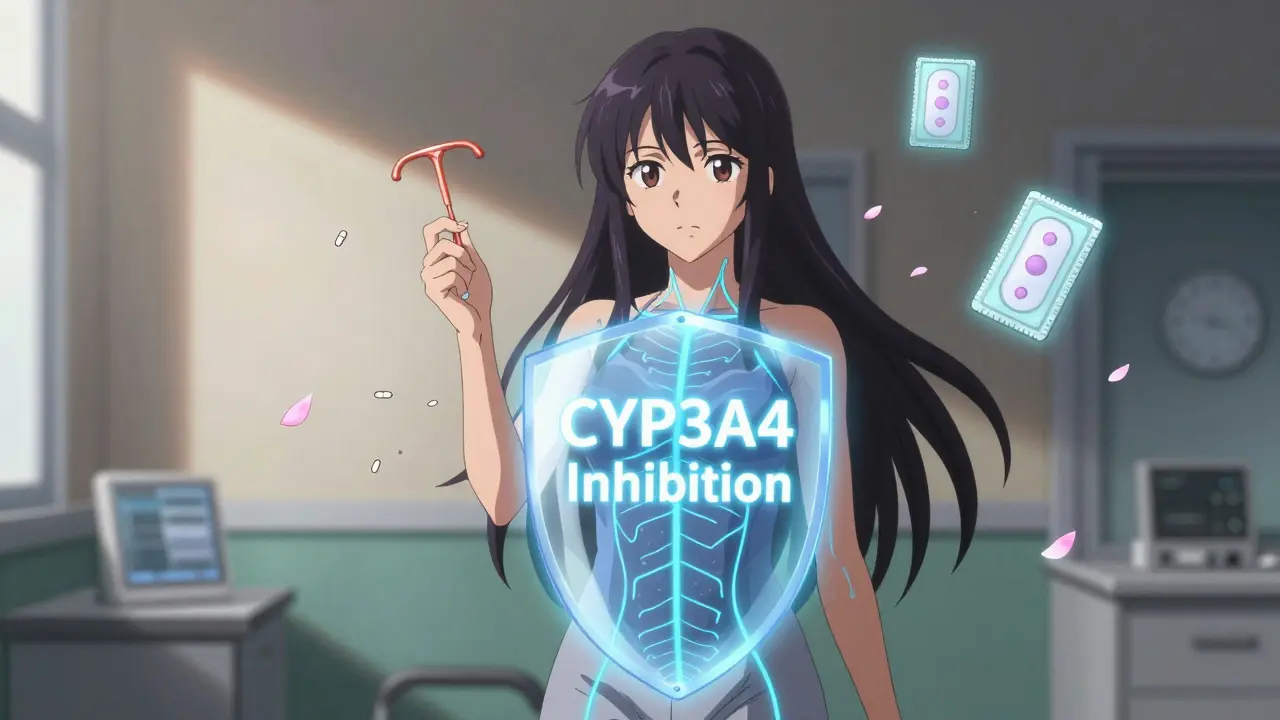
December 9, 2025 AT 14:27While the empirical evidence supporting chronopharmacological interventions is increasingly robust, the implementation of standardized temporal dosing protocols remains contingent upon the integration of validated circadian biomarkers into clinical decision support systems. Furthermore, the classification of medications into criticality tiers requires further granularity, particularly with regard to inter-individual variability in cytochrome P450 enzyme expression and renal clearance kinetics. Until such pharmacogenomic stratification is routinely incorporated into electronic prescribing workflows, the current dichotomous framework (high/moderate/low) risks oversimplification and potential therapeutic misalignment in heterogeneous patient populations.