How to Request a Lower-Cost Therapeutic Alternative Medication

Every year, millions of Americans skip doses, split pills, or don’t fill prescriptions because they can’t afford their meds. You’re not alone if you’ve stared at a $500 co-pay for a pill that’s supposed to keep you alive-and wondered if there’s another way. The good news? There’s a proven, safe, and often overlooked option: therapeutic alternative medication.
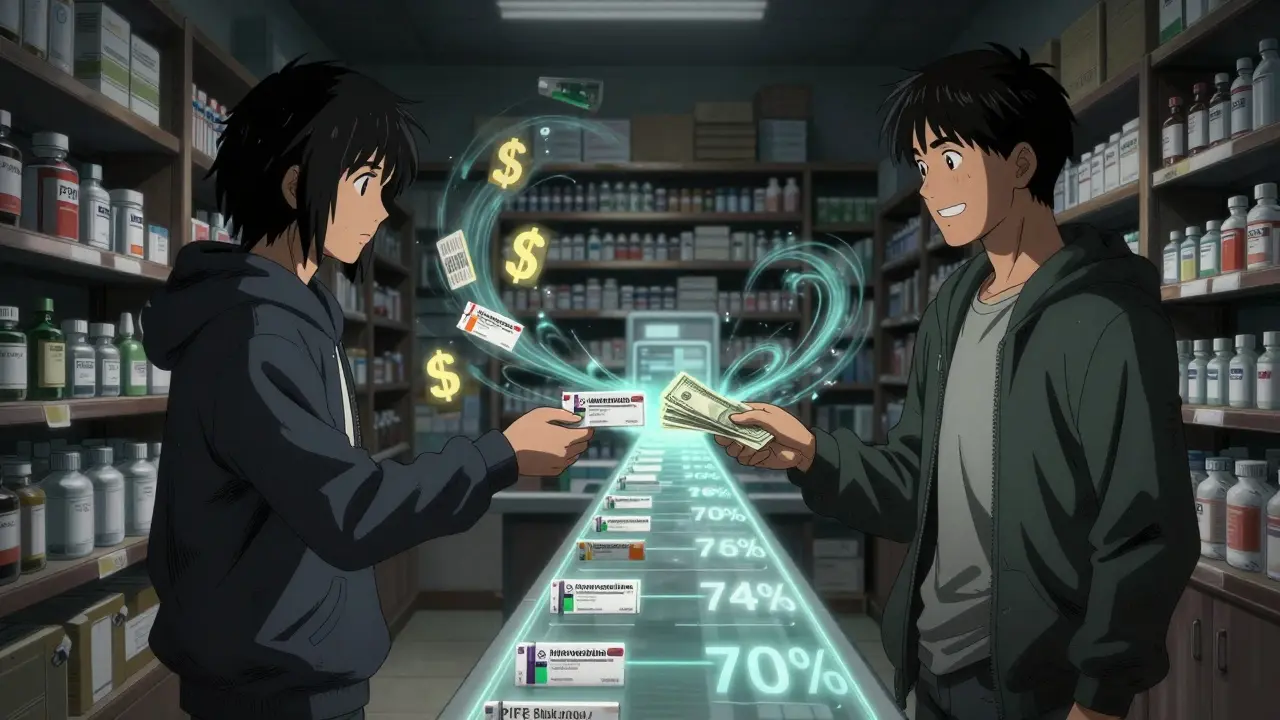
Therapeutic interchange isn’t about swapping your drug for a cheaper version of the same thing. That’s generic substitution. This is different. It’s when your doctor switches you from one medication to another that works the same way in your body-but costs a fraction. Think of it like trading a luxury sedan for a reliable economy car that gets you to the same destination.
What Exactly Is a Therapeutic Alternative?
A therapeutic alternative is a different drug-often from the same class-that treats the same condition with similar effectiveness and safety. For example:
- Instead of esomeprazole (Nexium), you could take omeprazole (Prilosec). One costs $365 a year. The other? $15.
- Instead of Lyrica (pregabalin), your doctor might suggest gabapentin. Monthly savings: $435.
- Instead of Eliquis, you could switch to warfarin. That’s a $450 monthly drop in cost.
These aren’t random swaps. They’re backed by clinical studies showing comparable results. A 2017 study from Vanderbilt University found that switching to therapeutic alternatives didn’t hurt patient outcomes-but saved $17.77 per person per month. That adds up fast.
Not all drugs have alternatives. About 15% of specialty medications-like those for rare cancers or autoimmune diseases-don’t have a clinically similar substitute. But for common conditions like high blood pressure, diabetes, acid reflux, depression, and high cholesterol? Alternatives are everywhere.
Why Don’t Doctors Always Suggest This?
You might expect your doctor to bring this up. But most don’t. Why?
- They’re not trained to ask. Only 37% of providers routinely screen patients for cost concerns.
- They’re unsure of alternatives. Many doctors didn’t learn about therapeutic interchange in medical school.
- They worry about backlash. Some fear patients will think they’re cutting corners-or that the switch won’t work.
But here’s the truth: When patients ask, doctors respond. A 2023 survey found that 68% of patients who requested a therapeutic alternative got it. The biggest barrier? Not the science. Not the insurance. It’s the conversation.
How to Ask for a Lower-Cost Option (Step by Step)
Asking doesn’t mean you’re giving up on your health. It means you’re taking control. Here’s how to do it right.
- Start with the cost question. Don’t wait for your doctor to ask. Say: “I’m having trouble affording this prescription. Are there cheaper options that work just as well?”
- Do your homework first. Go to GoodRx and search your medication. Look at the cash price-not the insurance price. You might be shocked. For example, 30 days of atorvastatin (generic Crestor) costs $12 at Walmart. The brand-name version? $400.
- Bring a specific suggestion. Don’t just say, “Can I get something cheaper?” Say: “Could I try omeprazole instead of esomeprazole? I saw it’s the same class and costs way less.”
- Ask about 90-day supplies. Many insurers charge the same copay for 90 days as they do for 30. That’s a 25% savings just by changing the refill schedule.
- Check for patient assistance programs. Many drugmakers offer free or low-cost meds to people who qualify. Sites like NeedyMeds and RxAssist list them. You don’t need to be poor-many programs accept incomes up to $60,000 a year.
One patient switched from Jardiance to metformin and saw her blood sugar spike. She went back to her doctor, explained the issue, and they found a different alternative-semaglutide-that worked. She’s now paying $20 a month instead of $700. That’s the power of persistence.

What to Do If Your Doctor Says No
If your doctor says, “This is the best option,” don’t give up. Ask why. Then ask for evidence.
Here are five common responses-and how to reply:
- “This is the most effective.” → “Can you show me the studies comparing it to [alternative]?” Many drugs in the same class have head-to-head trials showing no difference.
- “I’ve never tried that.” → “I found a 2022 American College of Physicians guideline that says [alternative] is equally safe for [condition]. Can we review it together?”
- “Your insurance won’t cover it.” → “Can we request a tiering exception? CMS requires them to respond within 72 hours for urgent cases.”
- “It’s not on our formulary.” → “Can you prescribe it anyway? I’ll pay out-of-pocket if needed.”
- “I don’t want to risk your health.” → “I understand. But I can’t afford this. What’s the worst that could happen if we try it for 30 days and monitor?”
Many doctors will reconsider once they see you’re informed and serious. A 2024 study found that patients who brought printed guidelines or GoodRx printouts were 3 times more likely to get their request approved.
When Therapeutic Alternatives Won’t Work
Not every drug has a safe substitute. This is especially true for:
- Biologics (like Humira, Enbrel, or Taltz) - these are complex proteins made in living cells. There are no true generics yet.
- Specialty cancer drugs - even small differences in dosage or formulation can be dangerous.
- Medications with narrow therapeutic windows - like warfarin or lithium - where tiny changes can cause side effects.
If you’re on one of these, therapeutic interchange isn’t the answer. But you still have options:
- Ask about manufacturer coupons or patient assistance programs.
- Check if your insurer offers a step therapy exception.
- Apply for nonprofit co-pay assistance-groups like the HealthWell Foundation help with over 1,200 medications.
Real Savings, Real Stories
People are saving hundreds every month using therapeutic alternatives:
- A 68-year-old man switched from Plavix to generic aspirin for heart protection. Saved $420/month.
- A woman with depression switched from Lexapro to generic escitalopram. Paid $5 instead of $180.
- A diabetic patient switched from Trulicity to metformin and added a low-cost GLP-1 alternative. Cut monthly cost from $900 to $50.
These aren’t outliers. They’re the result of asking the right question at the right time.
What’s Changing in 2025
Therapeutic interchange is getting easier. In October 2024, Medicare updated its rules to require all Part D plans to process therapeutic interchange requests within 72 hours if it’s urgent. In January 2025, Epic and Cerner-two of the biggest electronic health record systems-added new tools that automatically suggest cheaper alternatives when doctors write prescriptions.
Even better? The FDA is working on standardized criteria to define therapeutic equivalence across more drug classes. That means more clarity, fewer arguments, and more savings.
But don’t wait for the system to fix itself. The biggest driver of change is still you-asking, pushing, and refusing to pay more than you should.
Final Checklist: Your Action Plan
Before your next appointment, do this:
- Write down every medication you take.
- Go to GoodRx and note the cash price for each.
- Look up the generic or therapeutic alternative for each one.
- Find out if your drug is on the $4 list at Walmart, CVS, or Walgreens.
- Check NeedyMeds for patient assistance programs.
- Write down your question: “Can we talk about lower-cost alternatives?”
Therapeutic interchange isn’t a loophole. It’s a medical standard. You have the right to safe, effective care that doesn’t bankrupt you. Use it.
Can I switch to a therapeutic alternative without my doctor’s approval?
No. You must have your doctor approve any medication change. Even if a drug is cheaper or available over the counter, switching without medical guidance can be dangerous. Your doctor needs to evaluate whether the alternative is safe for your specific health conditions, other medications, and lab results.
Are therapeutic alternatives as safe as brand-name drugs?
Yes-when chosen correctly. Therapeutic alternatives are selected based on clinical trials showing they work similarly in the body. For example, multiple studies show that omeprazole and esomeprazole have nearly identical effects on stomach acid. The FDA requires that generic and therapeutic alternatives meet the same standards for purity, strength, and performance. The main difference is cost, not safety.
What if my insurance won’t cover the alternative?
Your doctor can file a tiering exception request. For Medicare Part D, this must be processed within 72 hours for urgent needs. For commercial insurance, ask your pharmacist to help you submit the form. Many insurers approve these requests if you show the alternative is clinically appropriate and cost-effective.
How long does it take to see results after switching?
It depends on the medication. For blood pressure or cholesterol drugs, you’ll typically see results in 2-4 weeks. For antidepressants or diabetes meds, it may take 4-8 weeks. Your doctor should schedule a follow-up to check how you’re doing. If the alternative isn’t working, you can switch back.
Can I use GoodRx with my insurance?
Usually not. GoodRx gives you the cash price, which is often lower than your insurance copay. You can choose to use GoodRx instead of your insurance, but you can’t combine them. If the GoodRx price is cheaper, pay cash. If your insurance copay is lower, use your plan. Always compare both before paying.
Why isn’t my doctor familiar with therapeutic alternatives?
Many doctors were trained before therapeutic interchange became a standard part of prescribing. Medical schools focus more on brand-name drugs, and pharmaceutical reps often promote expensive options. But that’s changing. More than 78% of primary care doctors now use therapeutic alternatives regularly. Don’t be afraid to bring up the topic-you’re helping them do their job better.
Are there any risks to switching medications?
When done under medical supervision, risks are very low. But some people respond differently to different drugs-even within the same class. For example, one person might do great on gabapentin but not on pregabalin. That’s why your doctor should monitor you after the switch. Never stop or switch meds on your own.
Can I get therapeutic alternatives for mental health meds?
Yes. Many antidepressants, antipsychotics, and anti-anxiety drugs have therapeutic alternatives. For example, sertraline (Zoloft) can often be swapped for citalopram (Celexa) or escitalopram (Lexapro). Savings can be $200-$500 per month. Always discuss mood changes or side effects with your doctor after switching.



Comments
Sam Black
December 22, 2025 AT 19:47Man, I wish my doctor in Melbourne had told me about this years ago. I was paying $400/month for a brand-name antidepressant until I found out generic escitalopram worked just as well for $8. I felt like an idiot for not asking sooner. This post is a godsend.
Aliyu Sani
December 23, 2025 AT 01:29Therapeutic interchange is the unspoken revolution in pharma. Most docs are trained to prescribe, not to interrogate cost structures. But the real power move? Bringing a GoodRx printout with the price difference circled. It’s not begging-it’s clinical advocacy. The system doesn’t change until you weaponize data.
Jeremy Hendriks
December 24, 2025 AT 23:15Let’s be real-this isn’t about alternatives. It’s about Big Pharma’s monopoly on human desperation. They patent the same molecule with a 0.3% structural tweak and call it ‘new.’ Then they charge $500. Meanwhile, your body doesn’t care if it’s esomeprazole or omeprazole-it just wants the damn acid to stop burning. The system is rigged. And you? You’re the only one who can break it.
Gabriella da Silva Mendes
December 26, 2025 AT 03:39OMG I’m so done with this 🤦♀️ I just want my Eliquis and I don’t care if it’s $800 a month!! I work hard and I deserve to not have to think about this!!! Why can’t they just make the good stuff cheaper?? Also why is everyone so obsessed with generics?? I’m not a lab rat 😭
Kiranjit Kaur
December 27, 2025 AT 08:47This is life-changing info!! 🙌 I’m from India and we’ve been doing this for years-generic metformin, gabapentin, even warfarin with regular INR checks. Why is this a revelation in the US? We need to spread this like wildfire. Share this with your aunt, your neighbor, your cousin who’s skipping pills. You’re not being cheap-you’re being smart. 💪
Sai Keerthan Reddy Proddatoori
December 28, 2025 AT 08:00They don’t want you to know this. Big Pharma owns the FDA. The FDA is just a shell. The real reason they don’t push alternatives? Because they’re paid to sell expensive drugs. Even your doctor gets kickbacks. I’ve seen it. They’ll say ‘this is best’ but they’re on the payroll. Stay vigilant. Don’t trust the system.
Kathryn Weymouth
December 30, 2025 AT 04:29I appreciate the practicality of this guide. However, I’d like to clarify a common misconception: therapeutic alternatives are not always interchangeable at the molecular level. For instance, while omeprazole and esomeprazole are both PPIs, esomeprazole is the S-isomer of omeprazole and has slightly different pharmacokinetics. Clinical equivalence does not always imply bioequivalence. It’s critical to review individual patient factors like CYP2C19 metabolism before switching.
Nader Bsyouni
December 31, 2025 AT 08:25So you’re telling me the entire medical-industrial complex is just a scam and all we need to do is ask nicely? Wow. Groundbreaking. I bet if I just whispered ‘please’ to my insulin pump it’ll lower the price. Meanwhile my blood sugar’s at 380 and my insurance denied my last claim because ‘it wasn’t medically necessary’ to have two vials a month. Thanks for the laugh
Julie Chavassieux
January 2, 2026 AT 07:12...I just cried reading this. I switched from Jardiance to metformin last year. My husband said I was being reckless. I lost 30 pounds. My A1c dropped from 9.2 to 5.8. I didn’t tell my doctor I was doing it on my own... I didn’t know I could. I’m scared now. What if I made a mistake? What if I die? But I’m so tired of paying $700 a month just to stay alive...
Herman Rousseau
January 3, 2026 AT 14:29Big shoutout to everyone who’s been saving lives with this info. Here’s a pro tip: When you ask your doctor for alternatives, say ‘I’m trying to stick to my budget so I can afford my rent and meds.’ That humanizes it. Doctors are people too. They want you to be healthy-not broke. Also, use GoodRx + pharmacy coupons together. Sometimes Walmart’s $4 list beats even the best insurance copay. You got this.
Vikrant Sura
January 4, 2026 AT 18:45Let’s not romanticize this. 80% of these ‘alternatives’ are just older generics with worse side effect profiles. You think gabapentin is the same as Lyrica? Try the neuropathic pain without the 30% efficacy drop. Then come back and tell me it’s ‘equivalent.’ This post is dangerously oversimplified. People die from unmonitored switches.
Candy Cotton
January 6, 2026 AT 14:35While the premise of therapeutic interchange is theoretically sound, it is not a panacea. The United States healthcare system operates under a complex regulatory framework governed by the FDA, CMS, and private payers. To suggest that a simple patient-initiated request can override these structures is not only naïve but potentially hazardous. Professional medical judgment must prevail over cost-driven decision-making.
Ajay Brahmandam
January 7, 2026 AT 14:56My dad switched from Crestor to generic atorvastatin and saved $380/month. He didn’t even notice a difference. I showed him this article and he said ‘why didn’t they tell me this before?’ I think the real problem isn’t the meds-it’s that nobody talks about money in doctor’s offices. We need to normalize asking. It’s not rude. It’s necessary.
jenny guachamboza
January 8, 2026 AT 23:47ok but what if the alternative gives you anxiety?? I switched to generic Lexapro and started having panic attacks?? and then my doctor said ‘it’s all in your head’?? and now i think they’re poisoning us with the cheap stuff?? i saw a video on tiktok about this and it said the fillers are different?? i’m scared to take anything now 😭
Tarun Sharma
January 9, 2026 AT 00:07Thank you for this comprehensive overview. The clinical rationale for therapeutic interchange is well-supported in peer-reviewed literature. I would recommend integrating this approach into routine primary care protocols, particularly in high-cost medication regimens. Patient autonomy and cost-effectiveness are not mutually exclusive.