How Lower Generic Drug Prices Improve Patient Adherence and Cut Healthcare Costs

When a doctor prescribes a medication, the goal is simple: the patient takes it as directed. But for millions of people, that doesn’t happen-not because they don’t care, but because they can’t afford it. The gap between what a drug costs and what a patient can pay directly shapes whether they take their medicine. And the data is clear: when generic drug prices drop, adherence goes up. When prices rise, people skip doses, delay refills, or skip pills entirely. This isn’t just about personal choices-it’s about lives, hospital stays, and billions in avoidable healthcare spending.
Why Cost Stops People from Taking Their Medicine
Out-of-pocket costs are the biggest barrier to medication adherence. It doesn’t matter if the drug is for high blood pressure, diabetes, or depression-if the copay is $75, many will skip it. A 2023 JAMA Network Open survey of over 2,100 adults found that nearly one in three (32.7%) admitted to not filling a prescription, skipping doses, or cutting pills in half to save money. That’s not laziness. That’s survival. The pattern is predictable. Every $10 increase in a patient’s copay leads to a 2-4% drop in adherence, according to a 2022 review in the Journal of Managed Care & Specialty Pharmacy. For drugs like GLP-1 agonists used in diabetes, each $10 rise in cost reduces the chance someone will stick with their treatment by 3.7%. That small change triggers bigger consequences: a 5.2% spike in emergency room visits among those who stop taking their meds. It’s not just about the price tag. It’s about surprise. Many patients don’t know how much a prescription will cost until they get to the pharmacy. A 2023 survey showed that 78% of people who’d skipped meds due to cost said they’d have filled the prescription if they’d known the real price ahead of time. That’s a system failure-not a patient failure.Generics Work Just as Well-And Cost Way Less
Generic drugs aren’t second-rate. They’re the exact same medicine, made with the same active ingredients, in the same strength and form as brand-name drugs. The FDA requires them to match brand-name drugs within 80-125% of their bioavailability-meaning they work the same way in your body. Yet, they cost 80-85% less. In 2022, generics made up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That’s $643 billion saved between 2009 and 2019, according to the Association for Accessible Medicines. And that savings translates directly into better adherence. Take statins-medications for lowering cholesterol. When Medicare Part D moved brand-name atorvastatin and rosuvastatin from a higher-cost tier to a lower one, adherence jumped by 5.9%. That’s not a small number. That’s thousands of people avoiding heart attacks and strokes because they could finally afford their meds. Another study looked at women taking aromatase inhibitors after breast cancer treatment. Those on brand-name versions had a 22.3% discontinuation rate. Those on generics? Only 17.8%. Adherence rates were 73.1% for generics versus 68.4% for brands. The difference? Cost. The brand-name version had a $100 copay. The generic? $10. One Reddit user, u/HeartHealthJourney, shared: “After my cardiologist switched me from brand-name Crestor ($75 copay) to generic rosuvastatin ($5 copay), I went from missing 3-4 doses weekly to perfect adherence for 11 months straight.” That’s not an outlier. That’s the norm when price drops.The Domino Effect of Non-Adherence
When people don’t take their meds, the consequences ripple through the system. Medication non-adherence causes up to 50% of treatment failures. It contributes to more than 100,000 preventable deaths each year in the U.S. And it costs the healthcare system between $100 billion and $300 billion annually, according to Magellan Health Insights. Think about it: someone with high blood pressure skips their pill because it’s too expensive. Their pressure stays high. A year later, they have a stroke. The hospital bill? $50,000. The rehab? Another $20,000. The lost wages? $30,000. The cost of the pill? $5 a month. Studies show that patients who stick to their meds have 15-20% fewer hospitalizations. That’s not just better health-it’s cheaper care. One study found that even though generic drugs increased drug spending slightly, overall healthcare costs dropped because fewer people ended up in the ER or hospital.
How Systems Are Changing to Help
The good news? Things are starting to shift. The Inflation Reduction Act of 2022 capped insulin at $35 a month for Medicare beneficiaries. By 2025, there will be a $2,000 annual cap on out-of-pocket drug costs for Medicare Part D users. That’s going to help 1.4 million people stay on their meds. Real-time benefit tools (RTBTs) are another game-changer. These systems show prescribers the actual cost of a medication before they write the script. In pilot programs, they’ve boosted adherence by 12-15%. One pharmacy program, Magellan’s inforMED, saw a 40% drop in care gaps and a 2:1 return on investment. That means for every dollar spent on the tool, two dollars were saved in avoided hospital visits. But tools alone aren’t enough. Patients still worry that generics aren’t as good. That’s where education matters. The FDA’s “It’s Okay to Use Generics” campaign has helped, but more needs to be done. Doctors need to talk about cost-not just as an afterthought, but as part of the treatment plan.What Still Doesn’t Work
Despite the evidence, some systems still make adherence harder. Tiered formularies that charge $100 for a brand-name drug and $10 for the generic still exist. Therapeutic duplication-giving patients two drugs that do the same thing-is still common and accounts for 20-30% of avoidable drug costs. And while generics are cheaper, they’re not always available. Some drugs still have no generic version, even after patents expire, thanks to legal delays or manufacturing bottlenecks. The FDA’s 2023 Generic Drug User Fee Amendments (GDUFA III) are trying to fix that. With $1.1 billion committed to speeding up approvals, over 1,500 new generics could hit the market by 2027. There’s also the issue of price gouging. From 2022 to 2023, the average price of over 4,200 drugs rose-48.7% of those increases outpaced inflation. Americans pay 256% more for brand-name drugs than people in Australia, Canada, Germany, or the UK. That’s not market efficiency. That’s a broken system.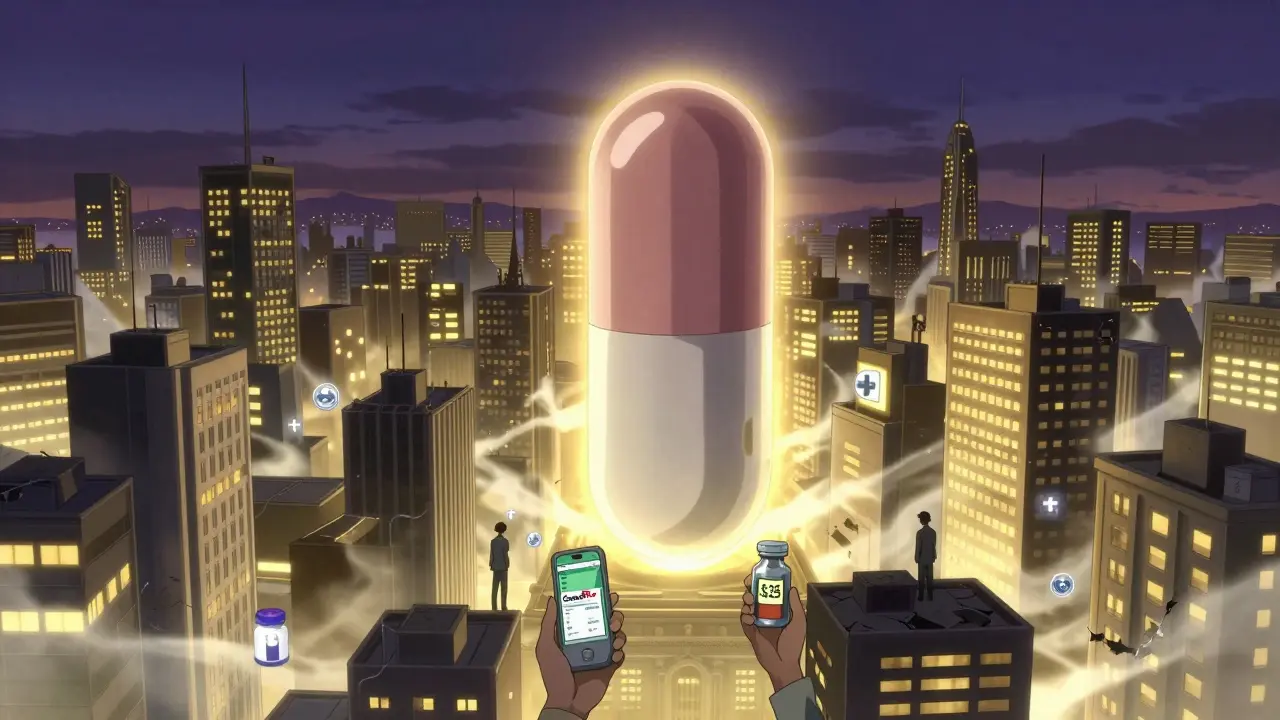
What Patients Can Do Today
You don’t have to wait for policy changes to take control. If you’re struggling to afford your meds:- Ask your doctor if a generic version is available.
- Use apps like GoodRx to compare prices at nearby pharmacies-sometimes the cash price is lower than your copay.
- Ask about patient assistance programs. Many drugmakers offer free or discounted meds for low-income patients.
- Request a 90-day supply. It’s often cheaper per pill and reduces the number of trips to the pharmacy.
- Speak up. Tell your doctor if cost is stopping you from taking your medicine. They can often switch you to a lower-cost option.
What Providers and Payers Should Do
Doctors and insurers need to treat cost as part of the treatment. Prescribing a $150-a-month drug without checking if the patient can afford it is like prescribing a pill with no instructions. It’s dangerous. Health systems should:- Integrate real-time cost tools into electronic health records so prescribers see prices before writing scripts.
- Train staff to discuss cost openly with patients-not as a taboo topic, but as a standard part of care.
- Use predictive analytics to flag patients at risk of non-adherence before they stop taking their meds.
- Move high-value medications (like those for diabetes or heart disease) to the lowest cost tier, regardless of brand status.
The Bigger Picture
Lower generic prices aren’t just a cost-cutting trick. They’re a public health strategy. When people can afford their meds, they stay healthier. Hospitals fill fewer beds. Emergency rooms see fewer avoidable cases. Families don’t lose income because a loved one ends up in the ICU. The data doesn’t lie: cheaper generics = better adherence = fewer deaths = lower costs. It’s a chain reaction, and it starts with a simple decision: let people afford what they need. The question isn’t whether we can afford to make generics cheaper. It’s whether we can afford not to.Are generic drugs as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also prove they work the same way in the body-within 80-125% of the brand’s bioavailability. Thousands of studies confirm they’re just as safe and effective. The only difference is the price-generics cost 80-85% less.
Why do some people still avoid generics?
Some believe generics are inferior because they look different or are cheaper. Others have had bad experiences with early generics, which were less reliable before stricter FDA rules in the 2000s. Misinformation and lack of education play a big role. But today’s generics are held to the same standards as brand-name drugs. The FDA’s “It’s Okay to Use Generics” campaign helps, but doctors need to reinforce this message every time they prescribe.
How much can I save by switching to a generic?
On average, you’ll save 80-85%. For example, brand-name Lipitor (atorvastatin) might cost $75 a month with insurance, while generic atorvastatin can be as low as $5-$10. For chronic conditions like high blood pressure or diabetes, that’s hundreds of dollars saved each year. Some patients report saving over $1,000 annually just by switching to generics.
Can I ask my doctor to switch me to a cheaper drug?
Absolutely. You have the right to ask. Say something like, “I’m having trouble affording this prescription. Is there a generic version or another medication that’s less expensive but just as effective?” Doctors are more likely to help if you bring it up early. Many now use real-time cost tools and can suggest alternatives on the spot.
What if my insurance doesn’t cover the generic?
That’s rare, but it can happen if the generic isn’t on your plan’s formulary. Ask your pharmacist to check if a different generic version is covered. You can also ask your doctor to submit a prior authorization request. If all else fails, use GoodRx or similar apps to find the lowest cash price. Sometimes, paying out of pocket is cheaper than your insurance copay.
Does this apply to all types of medications?
Yes-especially for chronic conditions like high blood pressure, cholesterol, diabetes, asthma, depression, and thyroid disorders. Studies show the strongest link between cost and adherence in these areas. For some life-saving drugs like HIV medications, adherence stays high even with high costs, but that’s the exception. For the vast majority of prescriptions, price still drives behavior.






Comments
vivian papadatu
January 31, 2026 AT 13:10Every time I see someone say generics are "not as good," I think of my mom who went from missing her blood pressure meds to taking them perfectly after switching to generic lisinopril. The only thing that changed was the price - not the pill. She’s been stable for three years now. This isn’t theory. It’s real life.
And yes, I know some people think the FDA is lazy. But if generics were dangerous, we’d be seeing mass poisonings. We’re not. We’re seeing preventable strokes and bankruptcies.
Doctors need to stop acting like cost is a personal failing. It’s a systemic one. And we’re all paying for it - in ER bills, in lost wages, in grief.
Naresh L
February 1, 2026 AT 15:55In India, we understand this better than most. A man with diabetes here doesn’t choose between insulin and groceries - he chooses between insulin and his child’s school fees. The brand-name drugs are myths in rural clinics. Generics aren’t a preference - they’re survival.
Yet even here, misinformation lingers. Some believe that because a pill is cheaper, it must be weaker. I’ve seen grandmothers break tablets in half because they think that’s what the doctor meant by "take one daily." It’s tragic. Education needs to meet people where they are - not where we wish they were.
Sami Sahil
February 1, 2026 AT 23:31bro i used to skip my metformin because it was $60 a month. then i switched to generic and it was $8. i didn’t even know that was possible. now i take it like clockwork. i’m not even trying to be healthy - i just don’t wanna feel like garbage after eating rice. thanks for reminding me that i’m not the only one who’s been stuck in this trap.
ps: goodrx saved my life. literally. i used it to find a pharmacy 3 blocks away that had it for $3. i cried.
pps: why do pharmacies still make you wait 20 mins to check price? it’s 2025.
franklin hillary
February 2, 2026 AT 14:24Let’s cut through the noise - this isn’t about healthcare. It’s about capitalism. Companies make billions off people’s suffering. They patent a drug for 20 years, then sit on it while generics wait. Then they tweak the pill slightly and relaunch it as "new and improved" - same active ingredient, 10x the price.
And we act surprised when people skip doses? No. We act surprised when they don’t die.
Generics aren’t a compromise. They’re the default. The brand names are the anomaly. The FDA doesn’t approve them because they’re cheap - they approve them because they’re identical. Stop acting like it’s a miracle that a $5 pill works the same as a $75 one. It’s science. Not magic.
And if you still don’t believe it? Take your brand-name statin. Crush it. Mix it with water. Drink it. Then take the generic. Drink it. Now tell me you can taste the difference. I’ll wait.
Bob Cohen
February 3, 2026 AT 08:33Oh wow. A whole article about how people can’t afford medicine. Shocking. I thought it was just me who had to choose between insulin and my kid’s braces.
Real talk: the system is rigged. The same people who scream about "personal responsibility" are the ones who profit when you skip your meds. And now they want to pat themselves on the back for capping insulin at $35? That’s like giving a drowning man a life jacket made of tissue paper.
Meanwhile, my cousin’s mom died last year from uncontrolled hypertension. Her copay went up $20. She skipped doses. Two months later - stroke. Hospital bill: $87,000. The pill? $6 a month.
So yeah. Let’s keep pretending this is about choice. I’ll be over here, laughing at the irony.
June Richards
February 3, 2026 AT 21:19Ugh. This is why I hate the left. You all act like drug companies are the villains, but what about the people who abuse the system? My cousin got 12 different prescriptions for the same thing - all generics - and sold them on the street. So now we’re rewarding cheaters with lower prices? Brilliant.
And don’t get me started on GoodRx. It’s just a middleman that screws over pharmacies. I’ve seen local pharmacies go under because of it. You think this is helping? It’s just shifting the pain.
Also, generics are often made in China. You really trust that? I mean, come on.
Lu Gao
February 4, 2026 AT 23:18Actually, I think this whole article is oversimplified. Yes, generics are cheaper - but they’re not always better. I had a friend who switched from brand-name Lexapro to generic escitalopram and had a full-blown panic attack within a week. The FDA says they’re "bioequivalent" - but bioequivalent doesn’t mean identical. Our bodies are complex. Some people react differently to fillers, dyes, coatings - things that vary between manufacturers.
And let’s not pretend everyone has access to GoodRx or knows how to ask for a generic. Many elderly patients don’t even have smartphones. This isn’t a one-size-fits-all fix. It’s a band-aid on a hemorrhage.
Angel Fitzpatrick
February 5, 2026 AT 23:16Wake up. This isn’t about affordability. It’s about control. The FDA, Big Pharma, and the CDC are all in bed with the same shadow entities that run the pharmaceutical supply chain. Generics? They’re not cheaper - they’re *engineered* to be cheaper. The active ingredient is the same, yes - but the delivery system is altered. They’re designed to have a shorter half-life. You think that’s an accident?
And don’t believe the "80-85% cheaper" lie. That’s calculated using inflated brand-name prices. The real cost of manufacturing? $0.03 per pill. The price you pay? $75. The profit margin? 249,900%.
They’re not trying to help you. They’re trying to keep you dependent. The lower price is a trap. It makes you think you’re winning - while they restructure the entire system to extract more later.
Check the GDUFA III funding. $1.1 billion? That’s not to speed up approvals. That’s to consolidate the generic market under fewer manufacturers. Monopoly. That’s the real goal.
Nidhi Rajpara
February 7, 2026 AT 01:39Dear all, I am writing this with utmost respect. In my country, India, we have been using generic medicines for decades. The quality is regulated by CDSCO, and it is very strict. I have personally taken generic medicines for hypertension, diabetes, and thyroid. All have worked well.
However, I have noticed that in the United States, patients often do not follow the prescribed dosage. They take medicine only when they feel symptoms. This is not due to cost - this is due to lack of discipline.
Also, I have seen many patients who do not understand the difference between brand and generic. They think generic means old or expired. This is a cultural issue, not a pricing issue.
Please educate patients. Not just about cost - but about adherence. Thank you.
Chris & Kara Cutler
February 7, 2026 AT 22:04My husband’s cholesterol meds went from $80 to $6. We cried. Then we bought pizza. 🍕❤️
Generics = freedom. No more skipping. No more guilt. Just pills and peace.
PS: GoodRx is my best friend.
Donna Macaranas
February 8, 2026 AT 05:15I used to think this was just a "rich vs poor" issue. Then my neighbor, a retired teacher on fixed income, told me she was cutting her metformin in half because she couldn’t afford the copay. She didn’t want to be a burden. I didn’t know. No one talks about this.
It’s not just about money. It’s about dignity. No one should have to choose between medicine and heat in winter. We’re better than this. We just need to act like it.
Rachel Liew
February 9, 2026 AT 13:00i had a friend who died because she couldn’t afford her blood thinner. she skipped doses for 3 months because the copay jumped from $15 to $75. no one knew. she didn’t want to be a bother.
her name was maria. she was 52.
we need to talk about this. not just in articles. in our kitchens. at dinner. with our doctors.
it’s not just a policy problem. it’s a human one.