Benzodiazepine Tapering: Safe Strategies to Reduce Dependence

Stopping benzodiazepines cold turkey can be dangerous. For people who’ve been taking them daily for months or years, sudden discontinuation can trigger seizures, panic attacks so severe they feel like heart attacks, hallucinations, or even delirium. The good news? You don’t have to quit all at once. A slow, guided benzodiazepine tapering process can help you break free from dependence without risking your safety.
Why Tapering Is Necessary
Benzodiazepines like Xanax, Valium, and Klonopin work by calming overactive brain signals. That’s why they help with anxiety, insomnia, and seizures. But after regular use-especially beyond four to six weeks-your brain adapts. It starts relying on the drug to stay balanced. When you stop, your brain is left scrambling. That’s withdrawal. The 2024 Joint Clinical Practice Guideline, developed by 10 major medical societies, confirms that tapering is the only safe way to stop long-term use. Abruptly quitting after daily use for more than a month carries a 20-40% risk of severe withdrawal. For short-acting benzos like alprazolam (Xanax), the risk is even higher. That’s why guidelines now say: if you’ve been taking these drugs for more than a few weeks, don’t just stop. Plan a taper.How Slow Should the Taper Be?
There’s no single answer. The speed depends on how long you’ve been taking the drug, your dose, your age, and your overall health. But here’s what the evidence says:- If you’ve been using benzodiazepines for 2-8 weeks: taper over at least 2 weeks.
- For 8 weeks to 6 months: aim for 4 weeks or longer.
- For 6 months to a year: plan for at least 8 weeks.
- For more than a year: tapers of 6 to 18 months are often needed.
Choosing the Right Medication for Tapering
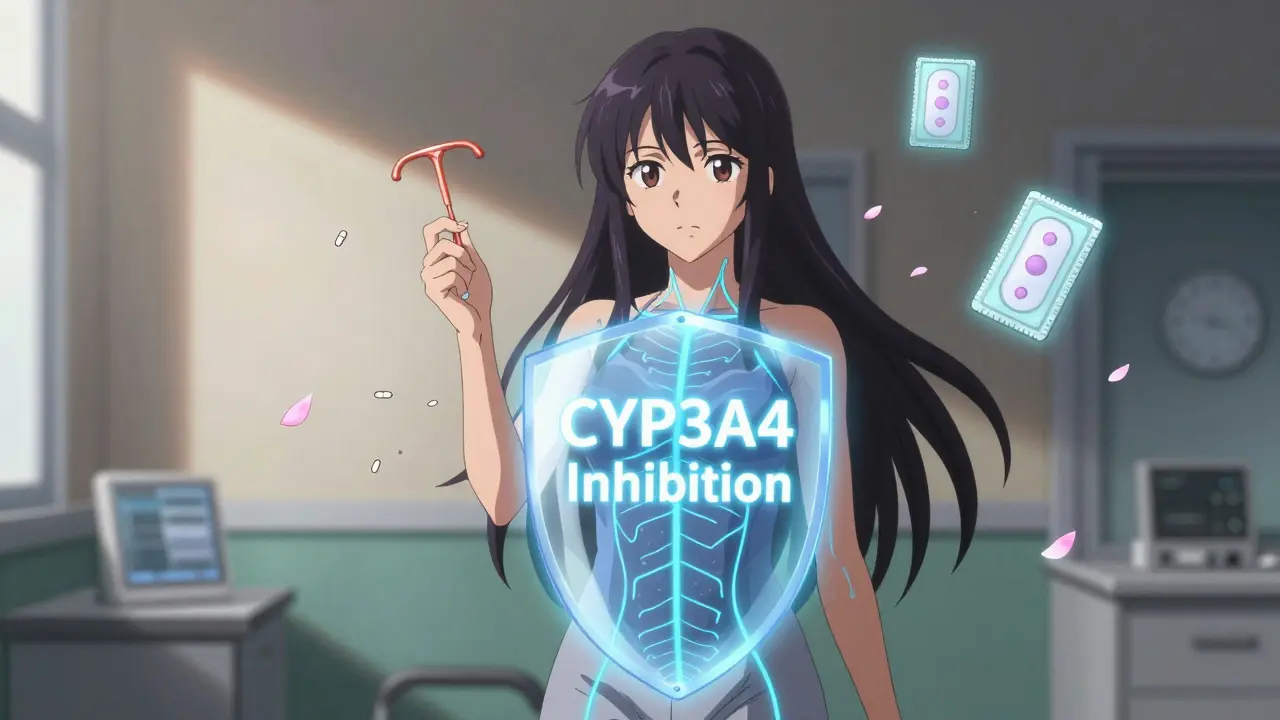
Not all benzodiazepines are the same. Some leave your body quickly. Others hang around longer, which makes withdrawal smoother.- Short-acting (alprazolam, lorazepam): These cause sharper withdrawal symptoms. If you’re on one of these, switching to a longer-acting option is often recommended.
- Long-acting (diazepam, clonazepam): These are preferred for tapering because they build up in your system and provide a steadier effect. Diazepam is the most commonly used for this purpose.
Three Main Tapering Approaches
There are three proven ways to taper:- Same medication taper: You reduce your current benzo slowly. Best for people on low doses or who’ve been on it for less than a year.
- Switch to diazepam: You change from your current benzo to diazepam first, then taper diazepam. This is the gold standard for long-term users or those on high doses. It’s the most predictable method.
- Adjunct medications: You use other drugs to help with symptoms during the taper. For example, antidepressants like SSRIs may help with anxiety. Sleep aids like trazodone or melatonin can help with insomnia. But these aren’t replacements-they’re supports.
Who Should Taper?
Tapering isn’t for everyone. But it’s strongly recommended for:- Older adults (65+): Benzodiazepines increase fall risk, confusion, and car accidents. The Beers Criteria lists them as potentially inappropriate for seniors.
- People with a history of substance use: Benzos can be misused. Tapering reduces dependency risk.
- Those with PTSD or chronic pain: Studies show benzos interfere with trauma therapy and don’t help long-term pain. The VA calls this a high-risk practice.
- Anyone on multiple benzos or combining them with opioids or stimulants: This combo increases overdose risk.
What Happens During Withdrawal?
Withdrawal symptoms aren’t the same for everyone. Some people feel fine. Others struggle. Common symptoms include:- Anxiety that feels worse than before you started
- Insomnia, even if you used the drug to sleep
- Tremors, muscle twitches, or headaches
- Sensory changes: buzzing in ears, sensitivity to light or sound
- Nausea, dizziness, or heart palpitations
Support Matters More Than You Think
Tapering isn’t just about pills. It’s about building new coping skills. People who succeed are those who get help.- Cognitive behavioral therapy (CBT): Proven to reduce anxiety without drugs. One 2024 JAMA Psychiatry study found that combining CBT with tapering led to a 68.3% success rate-nearly double the success of tapering alone.
- Peer support: Talking to someone who’s been through it helps. The VA now includes peer-support providers in tapering plans.
- Regular check-ins: Weekly or biweekly visits with your doctor are essential. They help catch problems early and adjust the plan.
Practical Tips for Success
Here’s what works in real life:- Use one doctor and one pharmacy. This prevents accidental double-dosing or diversion.
- Get prescriptions for only 1-2 weeks at a time. This forces you to check in regularly.
- Track your symptoms in a journal. Note sleep, anxiety levels, physical sensations. It helps you and your doctor see patterns.
- Don’t use alcohol or other sedatives during tapering. They make withdrawal worse.
- Keep your routine stable. Sleep, exercise, and meals matter more than ever during this time.
What If You Can’t Quit?
Some people try tapering but can’t get off completely. That’s okay. The goal isn’t always zero. It’s safety. If you’re on a low dose, your symptoms are stable, and you’re not at risk for falls or cognitive decline, staying on a minimal dose may be the best choice. The 2024 guidelines say: if alternatives have failed and the benefits clearly outweigh the risks, long-term low-dose use can be appropriate. This isn’t failure. It’s personalized care.The Future of Tapering
New tools are emerging. The NIH is funding a mobile app that tracks symptoms and suggests dose adjustments in real time. Early results show promise. In the next 3-5 years, tapering will become standard practice-not an afterthought. Veterans Affairs has already cut long-term benzo use by 23.7% since 2020 using structured protocols. States are following: 28 now require tapering plans for prescriptions longer than 90 days. The message is clear: you don’t have to live with dependence. With the right plan, support, and patience, you can reclaim your brain and your life.Can I taper off benzodiazepines on my own?
It’s not recommended. Tapering without medical supervision increases the risk of severe withdrawal, including seizures. Even if you feel fine, your body may be changing in ways you can’t detect. A doctor can adjust your plan based on symptoms, check for interactions, and rule out other conditions. If you’re in a rural area with limited access, telehealth and pharmacist-led programs can help fill the gap.
How long do withdrawal symptoms last?
Acute withdrawal usually lasts 1-4 weeks after your last dose reduction. For long-term users, symptoms like anxiety, sleep issues, or brain fog can linger for months-this is called protracted withdrawal. It’s not dangerous, but it’s frustrating. Most people notice steady improvement over 3-6 months. Patience and consistent routines are key. Avoid rushing the process; going too fast can make symptoms worse and longer-lasting.
Is diazepam (Valium) better than other benzos for tapering?
Yes, for most people on long-term therapy. Diazepam has a long half-life and builds up in your system, which creates a smoother decline in drug levels. This reduces the intensity of withdrawal compared to short-acting drugs like Xanax or Ativan. Switching to diazepam first, then tapering it slowly, is the most evidence-backed approach for doses over 6 months. It’s not about addiction-it’s about physics. Longer-acting drugs give your brain more time to adjust.
Can I use sleep aids or anti-anxiety meds during tapering?
Yes-but carefully. Non-addictive options like melatonin, trazodone, or certain SSRIs (like sertraline) can help manage symptoms. But avoid anything with sedative properties like zolpidem (Ambien) or other benzos. The goal is to build natural coping, not swap one dependency for another. Always discuss alternatives with your prescriber. Some people benefit from therapy-based tools like breathing exercises or mindfulness apps.
What if my doctor won’t help me taper?
You’re not alone. Many doctors still don’t know the latest guidelines. Bring printed copies of the 2024 Joint Clinical Practice Guideline or the Oregon Health Authority’s tapering protocol. Ask for a referral to a psychiatrist, addiction specialist, or clinical pharmacist. Veterans can access VA tapering programs. If you’re in the U.S., SAMHSA’s helpline (1-800-662-HELP) can connect you to local resources. Don’t give up-your health matters.


Comments
Ellen Calnan
November 21, 2025 AT 00:02God, I wish I’d known this five years ago. I tapered off Xanax cold turkey because I thought I was ‘strong enough’-ended up in the ER with heart palpitations that felt like my chest was being crushed. Took me six months to feel human again. Slow and steady isn’t sexy, but it’s the only way your brain doesn’t scream at you for months.
Don’t let anyone tell you it’s ‘just anxiety.’ Your nervous system remembers. And it holds grudges.
Andrew Montandon
November 21, 2025 AT 09:54YES. This is the most practical, non-judgmental guide I’ve ever read. So many doctors still treat tapering like a chore-not a medical necessity. I switched from lorazepam to diazepam after reading this exact protocol. My tremors dropped by 80% in two weeks. Seriously, print this out and give it to your prescriber. If they don’t get it, find someone who does.
Also-journaling. Do it. Even if you hate writing. Write one sentence a day. It saves your sanity.
Derron Vanderpoel
November 22, 2025 AT 06:19so i tried the diazepam switch but my doc just gave me a script and said ‘good luck’… i ended up feeling like i was walking through molasses for 3 months. brain fog so thick i forgot my own phone number. not cool. you need more than a pill-you need someone who actually gets it.
Richard Risemberg
November 22, 2025 AT 06:37Let me tell you about my cousin who tapered over 14 months. He was on 10mg of clonazepam daily for 11 years. Started at 5% reductions every 28 days. Used CBT, walked 5 miles every morning, and tracked his sleep with an app. He didn’t just quit benzos-he rebuilt his life.
Now he’s a yoga instructor. No irony. He says the anxiety he felt during tapering? It was the same anxiety he’d been numbing for a decade. Once it surfaced, he finally had to face it. And he did.
Don’t think of this as withdrawal. Think of it as your brain coming home.
river weiss
November 24, 2025 AT 01:44For anyone considering tapering: please, please, please do not attempt this without a clinician who specializes in psychiatric medication management. Many general practitioners have never read the 2024 Joint Clinical Practice Guideline. They’re still operating on 2010-era assumptions.
Ask for a referral to a psychiatrist who treats benzodiazepine dependence as a neurological condition-not a moral failing. Look for someone who mentions ‘half-life,’ ‘GABA receptor downregulation,’ or ‘protracted withdrawal’ in their intake forms.
If they don’t use those terms, they’re not qualified. Your brain is not a light switch.
seamus moginie
November 24, 2025 AT 03:44my mate in dublin did this last year-switched from klonopin to diazepam, went from 4mg to 0.5mg over 18 months. he said the worst part was people telling him to ‘just chill out’ like it was a bad mood. he cried every week for six months. but now? he’s running marathons. no meds. no panic. just breath.
if you’re reading this and scared? you’re not alone. just keep going. one day at a time.
Dion Hetemi
November 24, 2025 AT 10:11Let’s be real-this whole tapering thing is just Big Pharma’s way of keeping you dependent longer. Diazepam? It’s still a benzo. You’re just swapping one addiction for another with a longer shelf life. The real solution is therapy, not more pills. Why not just go cold turkey and get it over with? I’ve seen people do it and come out stronger.
Also, who even wrote this? Sounds like a drug rep wrote it with a thesaurus.
Sam Reicks
November 25, 2025 AT 00:05they dont want you to quit because the government makes billions off benzos and the hospitals get paid for withdrawal stays and the pharma companies own the doctors and the FDA is just a front for the drug lords and if you taper slow they can keep billing you for monthly visits and youll never be free and the real cure is hemp oil and a tinfoil hat and drinking rainwater
also i think my neighbor is a cia agent and he puts something in my coffee
Joe Durham
November 26, 2025 AT 19:15I’m not a doctor, but I’ve watched my sister go through this. The worst part wasn’t the physical stuff-it was the loneliness. People didn’t understand why she couldn’t just ‘snap out of it.’
She started a small online group for people tapering. Just 12 people. They shared journal entries, bad days, wins. One woman posted a photo of her first coffee without shaking. That’s the moment I knew: this isn’t about pills. It’s about reclaiming your quiet moments.
Be gentle with yourselves.
Kara Binning
November 28, 2025 AT 03:24As an American woman who has survived trauma, I find it absolutely disgraceful that our medical system treats benzodiazepine dependence like a minor inconvenience. We are not broken. We are not weak. We are survivors who were given a temporary lifeline-and then abandoned when we needed help to swim.
Why is it that when a man says ‘I need help,’ he gets a taper plan? When a woman says it, she gets labeled ‘hysterical’ and prescribed more pills?
This isn’t medicine. It’s misogyny with a prescription pad.
Brian Rono
November 29, 2025 AT 17:31Let me cut through the fluff: this guide is 90% correct, but it ignores the elephant in the room-most people who taper don’t succeed. The 68.3% success rate? That’s with intensive therapy, weekly check-ins, and a therapist who doesn’t charge $300/hour. For most working-class people? That’s a fantasy.
Also, diazepam isn’t magic. It’s just longer-acting. Your brain still rewires. You still suffer. And if you’re on a tight budget? Good luck finding a provider who won’t ghost you after two visits.
Stop romanticizing tapering. It’s hard. It’s messy. And it’s not for everyone.
Michael Petesch
November 29, 2025 AT 20:23While the clinical recommendations here are sound and well-supported by the 2024 guidelines, I would urge caution regarding the emphasis on diazepam as the universal standard. While its pharmacokinetic profile is advantageous, it is not universally accessible-particularly in regions with limited formulary coverage or where generic availability is inconsistent.
Furthermore, the assumption that all long-term users benefit from a switch ignores individual neurobiological variability. Some patients exhibit paradoxical reactions to diazepam, including increased anxiety or disinhibition. A one-size-fits-all approach, even one grounded in evidence, risks overlooking patient-specific phenotypes.
Personalized medicine in tapering is not a buzzword-it is a necessity.
Dana Dolan
December 1, 2025 AT 17:58my doc said i could taper in 6 weeks. i did. i cried for 11 days straight. i thought i was losing my mind. then i found this post. i switched to diazepam and slowed down. now i’m at 1mg. still not zero. but i sleep. i laugh. i don’t feel like i’m drowning.
you don’t have to be ‘cured’ to be free.