Dangerous Hyperkalemia from Medications: Cardiac Risks and Treatment
Hyperkalemia Risk Calculator
Your Risk Factors
This tool helps you understand your risk of dangerous hyperkalemia (high potassium) from common medications. Based on your inputs, it estimates your risk level and shows critical action steps.
Your Hyperkalemia Risk Assessment
Critical Action Steps
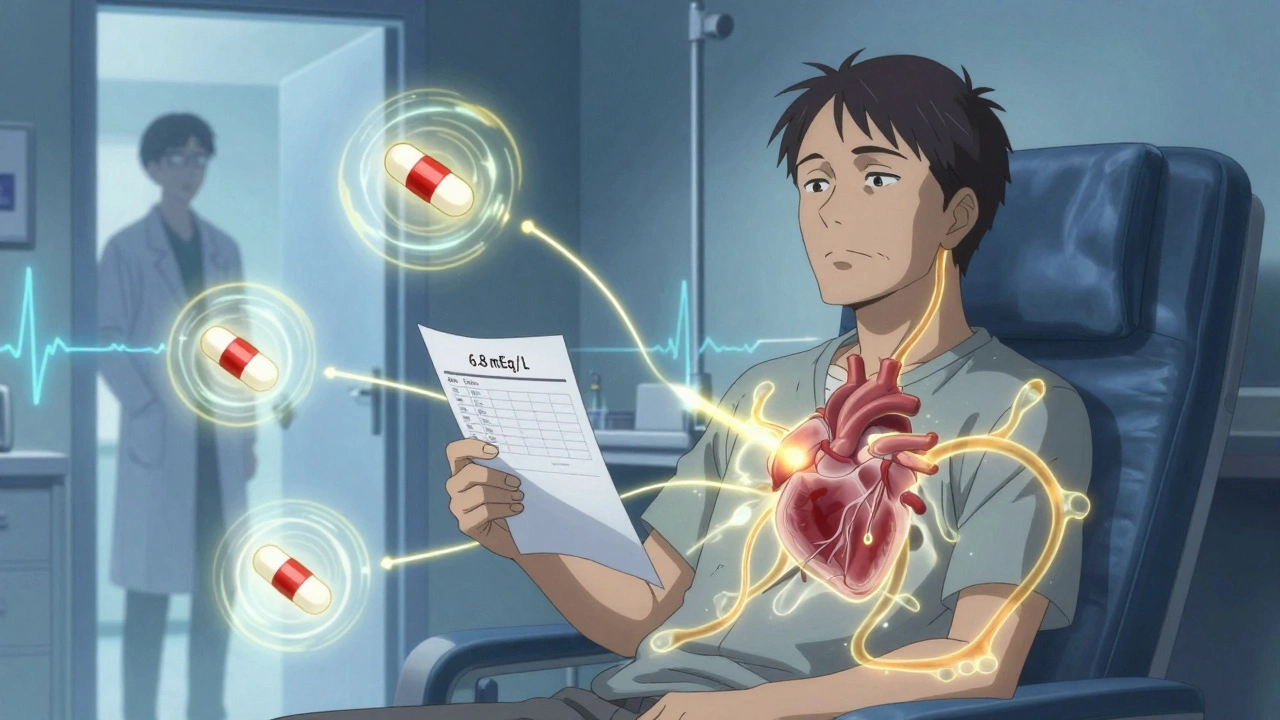
When you take a pill to lower your blood pressure or protect your kidneys, you expect it to help-not hurt. But for many people on common heart and kidney medications, a silent danger is building up in their blood: too much potassium. This isn’t just a lab number. It’s a ticking time bomb for your heart. Hyperkalemia-when potassium levels climb above 5.5 mEq/L-can cause your heart to flutter, skip beats, or stop entirely. And it’s often caused by the very drugs meant to save your life.
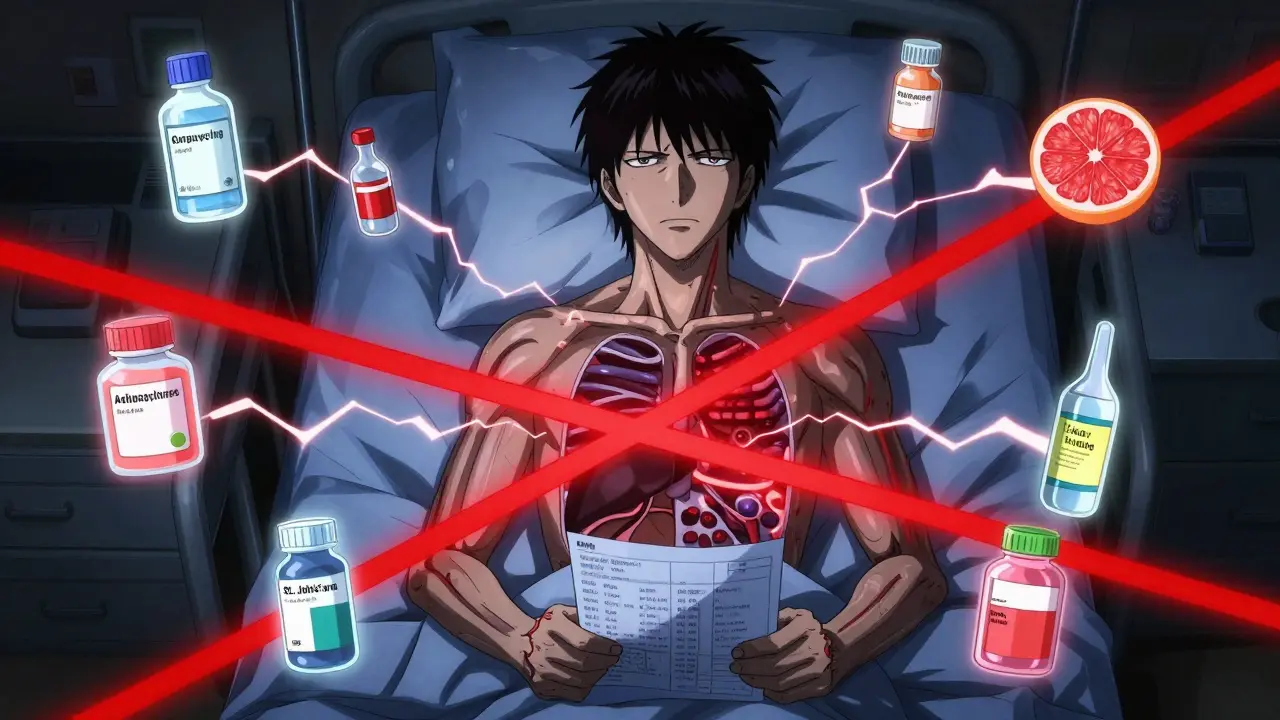
How Medications Turn Potassium Into a Threat
Potassium is essential. It helps your muscles contract, including your heart. But when levels rise too high, your heart’s electrical system goes haywire. The problem isn’t usually what you eat. It’s what you take. Drugs like ACE inhibitors (lisinopril), ARBs (losartan), and mineralocorticoid antagonists (spironolactone) are lifesavers for people with high blood pressure, heart failure, or chronic kidney disease. But they block the body’s natural way of getting rid of potassium. The result? Potassium builds up.And it gets worse when these drugs are combined. Taking spironolactone with an ACE inhibitor and a common antibiotic like co-trimoxazole can raise your risk of sudden death by more than five times. People with kidney problems, diabetes, or who are over 65 are especially at risk. Even mild kidney decline-a glomerular filtration rate under 60-can turn a safe dose into a dangerous one.
What makes this so tricky is that you often won’t feel anything. No chest pain. No shortness of breath. Just a quiet rise in potassium. By the time symptoms like muscle weakness or irregular heartbeat show up, it’s already late. That’s why regular blood tests are non-negotiable if you’re on these medications.
The Heart Pays the Price
Your heart runs on electricity. Potassium helps control that rhythm. When levels climb past 5.5 mEq/L, the electrical signals start to misfire. At 6.0 mEq/L, your ECG begins to show warning signs: tall, pointed T-waves. By 6.5 mEq/L, the PR interval stretches out. At 7.0 mEq/L or higher, your QRS complex widens. Then comes the sine wave pattern-the last signal before your heart goes into ventricular fibrillation and stops.Studies show patients with hyperkalemia are far more likely to suffer heart attacks, dangerous arrhythmias, or die in the hospital compared to those with normal potassium. The American Heart Association calls this a direct threat to cardiac function. And it’s not rare. Among people taking RAAS inhibitors, 10 to 20% develop hyperkalemia. In hospitals, 1 to 10% of patients develop it during their stay. That’s thousands of preventable cardiac emergencies every year.
And here’s the cruel twist: the drugs causing this danger are the same ones that reduce your long-term risk of heart failure and death. So stopping them might save you from high potassium-but it could cost you years of life.
What to Do When Potassium Is Too High
If your potassium hits 6.5 mEq/L or higher-or if your ECG shows changes-this is an emergency. You don’t wait. You act.First: calcium gluconate. Given through an IV, it doesn’t lower potassium. But it protects your heart. Within minutes, it stabilizes the heart muscle, stopping dangerous rhythms. It’s the first line of defense when your heart is in danger.
Next: move potassium into your cells. This is done with insulin and glucose. Ten units of insulin with 25 grams of glucose (often given as a bag of D5W) will lower potassium by 0.5 to 1.5 mEq/L within half an hour. Albuterol, inhaled through a nebulizer, does something similar-another 0.5 to 1.0 mEq/L drop. These aren’t cures. They’re time-buyers.
Then: get the potassium out. Diuretics like furosemide help the kidneys flush it out. But if your kidneys are already weak, that won’t be enough. That’s where newer drugs come in.
The Game-Changers: Potassium Binders
For years, the only solution when hyperkalemia happened was to stop the heart medication. But that meant giving up protection against heart failure and kidney decline. Now, we have alternatives.Patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) are oral binders. They work in your gut, trapping potassium before it enters your bloodstream. You take them daily. Within hours, potassium drops by 0.4 to 1.0 mEq/L. Studies show that with these drugs, 86% of patients can stay on their RAAS inhibitors. Without them, nearly 40% had to stop because of mild hyperkalemia.
They’re not perfect. About 1 in 5 people get constipation. A smaller number get diarrhea. But compared to the risk of stopping life-saving drugs, the trade-off is worth it. The National Kidney Foundation now recommends these binders as first-line treatment for patients who need to stay on RAAS inhibitors.

Living With the Risk
If you’re on one of these medications, here’s what you need to do:- Get your potassium checked every 1 to 4 weeks, especially when starting or changing doses.
- Don’t take potassium supplements unless your doctor tells you to. That includes salt substitutes-many are pure potassium chloride.
- Watch your diet. While you don’t need to eliminate bananas or potatoes, aim for under 3,000 mg of potassium per day. A medium banana has about 400 mg. A cup of cooked spinach has 800 mg.
- Know the warning signs: muscle weakness, tingling, irregular heartbeat. If you feel them, get checked immediately.
- Ask your doctor about potassium binders if you’ve had even one episode of high potassium.
Many patients never get proper education on this. Only 15 to 20% receive formal dietary counseling. That’s a gap. You can’t rely on your doctor to bring it up. Be the one to ask: “Could my meds be raising my potassium? Should I be on a binder?”
The Bigger Picture
This isn’t just about one electrolyte. It’s about how we balance risk in modern medicine. We used to see hyperkalemia as a reason to stop treatment. Now we see it as a condition we can manage-so we don’t have to stop saving lives.By using potassium binders, we’re keeping patients on drugs that cut heart failure deaths by up to 30%. We’re preventing hospitalizations. We’re keeping people out of the ER. And we’re doing it without giving up the benefits of the medications that have changed how we treat heart and kidney disease.
The future isn’t about avoiding high potassium. It’s about controlling it-so you can keep taking what keeps you alive.
Can high potassium from medications cause a heart attack?
Yes. When potassium levels rise above 6.5 mEq/L, it disrupts the heart’s electrical signals, leading to dangerous arrhythmias like ventricular fibrillation, which can cause sudden cardiac arrest. Even lower levels can trigger heart attacks in people with existing heart disease. The American Heart Association confirms that too much potassium can damage the heart and lead to heart attack.
Which medications most commonly cause hyperkalemia?
The top culprits are RAAS inhibitors: ACE inhibitors (like lisinopril), ARBs (like losartan), and mineralocorticoid receptor antagonists (like spironolactone). Potassium-sparing diuretics (such as amiloride) also contribute. The risk spikes when these are combined-especially with antibiotics like co-trimoxazole or in patients with kidney disease.
How do potassium binders like Lokelma and Veltassa work?
They work in your digestive tract, not your bloodstream. These medications bind to potassium in your intestines and trap it, so it passes out in your stool instead of being absorbed. They start working within hours and can lower potassium by 0.4 to 1.0 mEq/L. This allows patients to stay on heart-protective drugs like ACE inhibitors without risking dangerous spikes.
Is it safe to keep taking blood pressure meds if I have high potassium?
Yes-if you’re using potassium binders. Stopping these medications can increase your risk of death from heart failure or kidney decline by up to 30%. New guidelines from the National Kidney Foundation and the American Heart Association now recommend continuing RAAS inhibitors and adding a binder, rather than stopping the drug. The binder manages the potassium; the medication protects your heart and kidneys.
How often should I get my potassium checked?
If you’re on ACE inhibitors, ARBs, or spironolactone, check every 1 to 4 weeks after starting or changing the dose. Once stable, every 3 to 6 months is usually enough. But if you have kidney disease, diabetes, or are over 65, stick to monthly checks. Many doctors skip this-but it’s the only way to catch hyperkalemia before it’s an emergency.
Can I lower my potassium naturally with diet alone?
Diet helps, but it’s rarely enough. Cutting back on high-potassium foods like bananas, potatoes, spinach, and oranges can reduce intake by 500-1,000 mg per day. But if your kidneys aren’t working well or you’re on RAAS inhibitors, your body still holds onto potassium. You can’t out-eat the effect of these drugs. Diet should be part of the plan, not the only solution.




Comments
Christian Landry
December 8, 2025 AT 12:36bro i was on lisinopril and didn't know my potassium was sky-high until i passed out at the grocery store 😅
turns out i was also using salt substitute because i thought it was 'healthy'... yeah that was dumb.
got put on Lokelma and now i'm fine. just check your levels ppl. it's not scary if you catch it early.
Katie Harrison
December 9, 2025 AT 02:22I appreciate the thorough breakdown-but I’m concerned that many patients, especially elderly ones, are never warned about this. My mother was on spironolactone for years, and no one ever mentioned potassium... until she had a near-fatal arrhythmia.
Doctors assume patients will 'know' to ask. They won’t. We need mandatory counseling when these scripts are written.
And yes-diet helps, but it’s like trying to bail out a sinking boat with a teaspoon.
Michael Robinson
December 10, 2025 AT 12:25so we give people medicine to save their heart
but that medicine can kill their heart
and now we give them another pill to fix the first pill
is this progress or just a loop?
Kathy Haverly
December 11, 2025 AT 06:17Of course the pharmaceutical companies love this. First they sell you the drug that causes the problem. Then they sell you the drug to fix it. Then they sell you the blood tests to monitor the problem they created.
It’s not medicine. It’s a business model wrapped in a lab coat.
And now they want you to believe this is ‘innovation’? Please.
Haley P Law
December 12, 2025 AT 00:39MY MOM JUST GOT DIAGNOSED WITH THIS AND I’M SCARED 😭
she’s 72, on lisinopril and spironolactone, and her potassium was 6.8...
they gave her calcium IV and now she’s on Lokelma
but what if it doesn’t work??
is she gonna die??
please tell me she’s gonna be okay
im crying right now
help
Andrea DeWinter
December 13, 2025 AT 11:24Hey I’m a nurse and I see this all the time
you don’t need to panic but you do need to act
if you’re on any RAAS inhibitor get your potassium checked within 2 weeks of starting
and if you’ve had one high reading talk to your doc about binders
they’re not magic but they’re life-changing
and yes your banana is fine but skip the salt substitute
you got this
Steve Sullivan
December 14, 2025 AT 13:35life is just a series of trade-offs isn’t it?
take the pill and risk your heart stopping
or stop the pill and risk your heart failing over time
we’re not fixing disease anymore
we’re just managing side effects of side effects
and calling it progress
maybe we need better drugs
or maybe we need to stop treating symptoms and start treating causes
just saying
George Taylor
December 14, 2025 AT 21:16...and yet, despite all this, no one talks about the fact that 80% of these cases are preventable if doctors actually monitored labs properly.
But why bother? It’s easier to write a new prescription than to follow up.
And the system rewards volume over vigilance.
So we’re all just playing Russian roulette with our electrolytes.
Great job, healthcare.
ian septian
December 15, 2025 AT 23:49Check potassium. Monthly at first. Then every 3 months.
Don’t skip it.
Ask for binders if needed.
Live longer.