Medication Coverage: What Your Insurance Really Pays For and How to Get It
When you pick up a prescription, medication coverage, the portion of your drug cost paid by insurance. Also known as drug benefits, it’s not a guarantee — it’s a negotiation between your plan, the pharmacy, and the manufacturer. Many people assume if a drug is FDA-approved, insurance will pay for it. That’s not true. Coverage depends on your plan’s formulary, which changes yearly, and whether your doctor jumps through hoops like prior authorization, a requirement where insurers demand proof before approving certain drugs. For drugs like levothyroxine or phenytoin — those with a narrow therapeutic index, where tiny dosage changes can cause serious harm — insurers often force you to use the brand-name version, even if the generic works fine.
Why? Because some plans have deals with drugmakers, or they fear lawsuits if a generic fails. But here’s the catch: generic drugs, medications that copy brand-name drugs after patents expire are just as safe and effective, as long as they pass FDA bioequivalence studies, tests proving they absorb the same way in your body as the brand. Still, you might get stuck paying more if your insurer doesn’t list the generic on their preferred list. And if you’re taking multiple meds, drug interactions, when one medication changes how another works in your body can suddenly make your coverage useless — like mixing St. John’s Wort with antidepressants or colchicine with antibiotics. These aren’t rare mistakes. They happen every day.
What you can do? Always ask your pharmacist to check your coverage before you pay. Request a copy of your plan’s formulary. If a drug gets denied, appeal — many people win on the second try. An annual medication review, a meeting with a pharmacist to check all your drugs for safety and necessity can uncover hidden gaps in coverage and cut out pills you don’t need. You’re not just paying for pills — you’re paying for access, clarity, and control. The system isn’t perfect, but knowing how it works gives you power. Below, you’ll find real guides on how to fight for coverage, spot dangerous interactions, understand why generics get flagged, and what to ask your doctor when insurance says no.
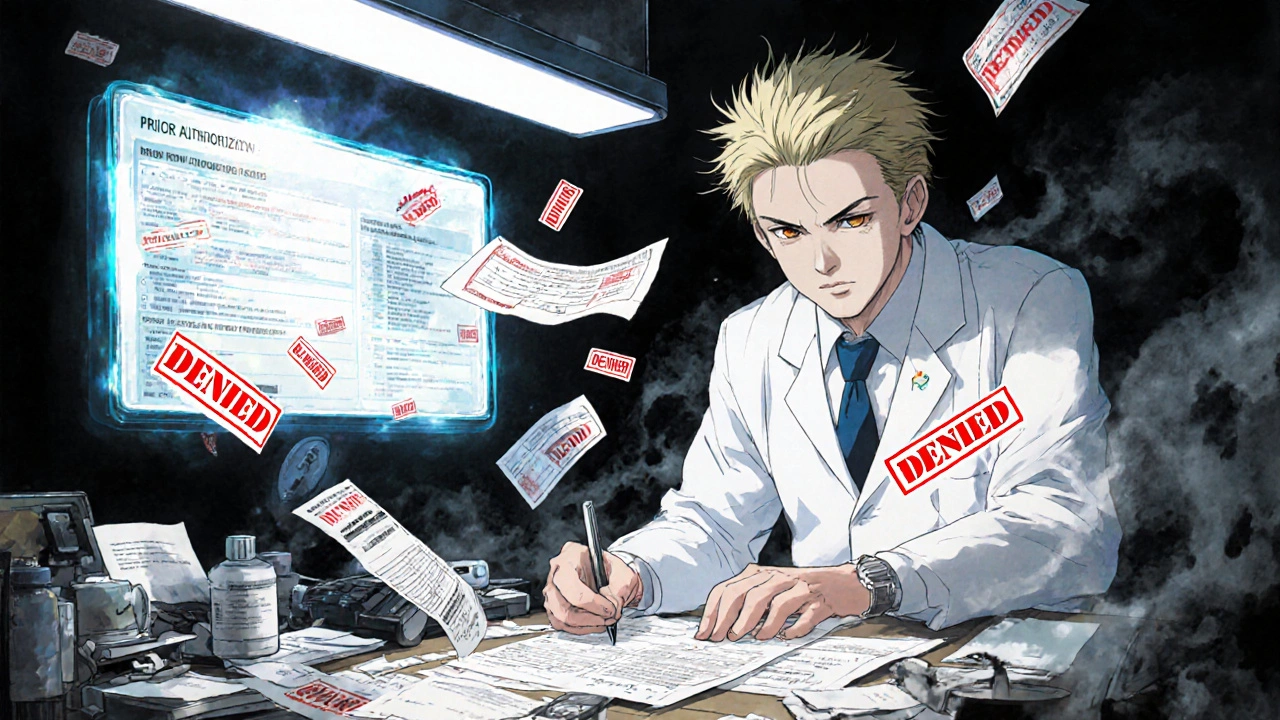
Prior Authorization Requirements for Medications Explained
Prior authorization is a common insurance requirement for certain medications. Learn how it works, why it's used, what to do if it's denied, and how to avoid delays in getting your prescription covered.