Postpartum Depression Treatment: Safe Antidepressants During Breastfeeding and What Side Effects to Watch For

Breastfeeding Medication Safety Checker
Select Your Antidepressant
Safety Rating
Key Information
Transfer rate: 0.5% to 3.2% of maternal dose in breast milk
Risk level: Low
Recommended by CDC, ACOG, and AAP for breastfeeding mothers
Baby Side Effects to Watch For
- Excessive sleepiness or difficulty waking to feed
- Poor sucking or refusal to nurse
- Unusual fussiness, crying, or irritability
- Changes in bowel movements
- Slow weight gain
Timing Tip: Take your medication right after nursing to minimize baby's exposure. This timing doesn't change overall effectiveness but reduces peak concentration in milk.
Postpartum depression isn’t just feeling tired or overwhelmed
It’s a real medical condition that affects about 1 in 8 new mothers. If you’re struggling with constant sadness, guilt, or numbness after giving birth - and it’s lasted more than two weeks - you’re not weak, broken, or failing. You’re sick. And you need treatment. The good news? There are safe, effective options that won’t force you to choose between healing and breastfeeding.
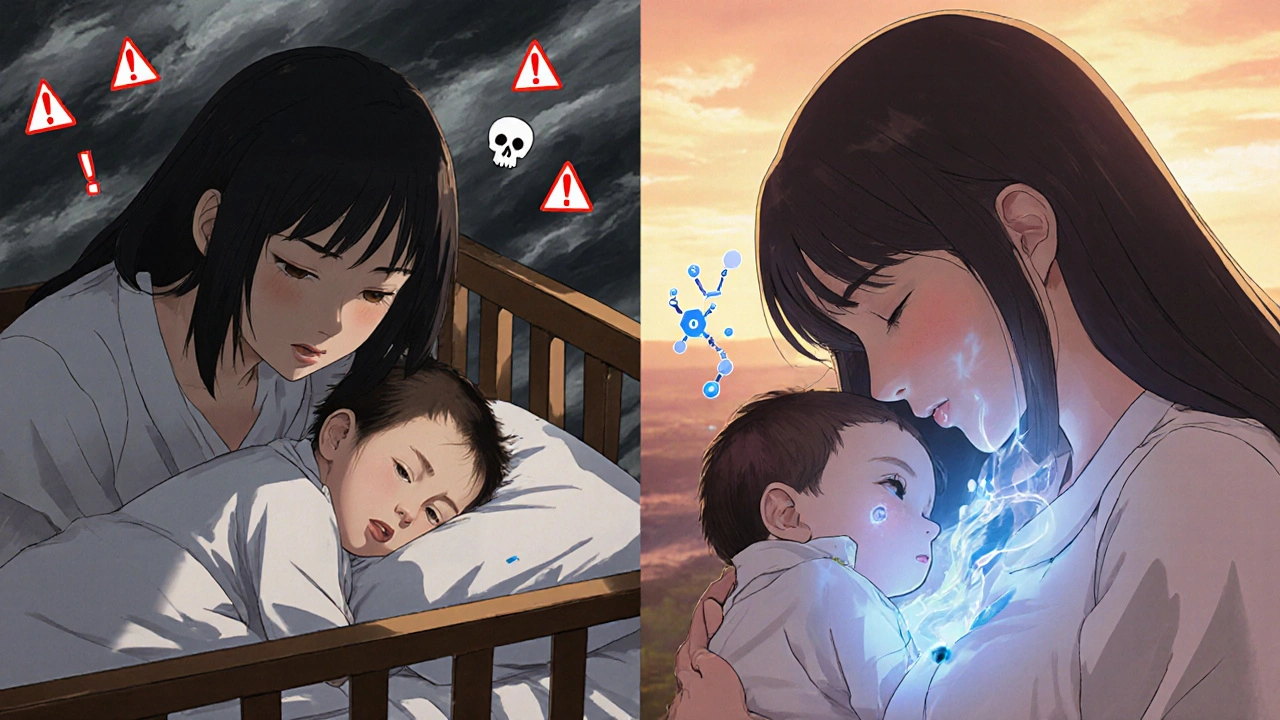
Why untreated depression is riskier than medication
Many moms worry that taking antidepressants while breastfeeding will harm their baby. But the truth is, the bigger danger is leaving depression untreated. When a mother can’t sleep, eat, or connect with her baby, the whole family suffers. Infants of mothers with untreated postpartum depression are more likely to have trouble bonding, delayed language development, and higher rates of anxiety later in childhood. The American College of Obstetricians and Gynecologists, the CDC, and the American Academy of Pediatrics all agree: the risks of untreated depression far outweigh the risks of most antidepressants in breast milk.
Not all antidepressants are the same during breastfeeding
When it comes to choosing a medication, the key is finding one with the lowest transfer into breast milk. The best-studied and safest options are SSRIs - selective serotonin reuptake inhibitors. Among them, sertraline is the gold standard. Studies show that only 0.5% to 3.2% of the mother’s dose ends up in breast milk. In over 90% of cases, babies have undetectable levels in their blood. Paroxetine is also low-risk, with transfer rates around 0.9% to 8.6%.
Other SSRIs like citalopram and escitalopram are moderate risk, with transfer rates of 3.5% to 8.9%. Fluoxetine? Avoid it if you can. It lingers in the body for weeks, and its active metabolite can build up in your baby’s system, reaching up to 30% of your blood levels. That’s why moms who switch from fluoxetine to sertraline often report their babies suddenly sleeping better, feeding more calmly, and crying less.
What about newer drugs like zuranolone?
In August 2023, the FDA approved zuranolone (Zurzuvae), the first oral pill specifically made for postpartum depression. It works fast - many women feel better in under two weeks. But here’s the catch: clinical trials required women to stop breastfeeding during treatment. The manufacturer doesn’t yet have enough data to say it’s safe. However, early estimates suggest the amount that gets into breast milk is very low - about 0.5% to 1.5% of the mother’s dose. Some experts believe it may be safe, but official guidelines still recommend pumping and dumping for a week after the last dose. If you’re considering zuranolone, talk to your doctor about whether the benefits outweigh the uncertainty.
Antidepressants to avoid during breastfeeding
Some medications carry clear risks. Doxepin has been linked to cases of infant apnea and blue spells, even at low doses. Bupropion (Wellbutrin) increases the risk of seizures in infants, especially those with a family history or neurological conditions. Fluoxetine is the worst offender in terms of accumulation - its long half-life means it stays in your baby’s system for days. Tricyclic antidepressants like amitriptyline are generally safe because they bind tightly to proteins in the mother’s blood, leaving little to pass into milk. But they can still cause drowsiness in newborns.
How to monitor your baby for side effects
Most babies show no signs at all. But in the first two to four weeks after starting an antidepressant, watch for:
- Excessive sleepiness or difficulty waking to feed
- Poor sucking or refusal to nurse
- Unusual fussiness, crying, or irritability
- Changes in bowel movements - diarrhea or constipation
- Slow weight gain
If you notice any of these, don’t panic. Call your pediatrician or a lactation consultant. Often, adjusting the dose or switching medications fixes the issue. One mom on a breastfeeding forum shared that her baby became extremely gassy and fussy on sertraline - until she switched the timing. Taking her pill right after nursing, instead of before, made all the difference.
Timing matters: When to take your pill
It’s not just about which drug you take - it’s when you take it. To minimize your baby’s exposure, take your antidepressant right after you finish a feeding. That way, the highest concentration in your blood happens when your baby is least likely to nurse again for several hours. For drugs like sertraline with a half-life of about 26 hours, this timing won’t change the overall effect - but it can reduce the peak amount your baby gets in each feeding.

What to expect when you start treatment
Antidepressants don’t work overnight. It usually takes three to four weeks before you feel any real improvement. That’s hard when you’re exhausted and overwhelmed. Don’t give up if you don’t feel better in a week. Keep taking it. Talk to your doctor if you’re not seeing progress after four weeks - they may adjust the dose or try a different medication. Abruptly stopping antidepressants increases your risk of relapse by three times. Recovery isn’t linear. Some days will be better than others. That’s normal.
Support is part of the treatment
Medication alone isn’t enough. Therapy - especially cognitive behavioral therapy (CBT) - works just as well as pills for mild to moderate postpartum depression. Many insurance plans now cover telehealth therapy for new moms. Support groups, whether online or in person, help too. Postpartum Support International has free peer-led groups for moms on antidepressants. Hearing other women say, “I felt the same way,” can be as healing as the medication itself.
Screening saves lives
Doctors are supposed to screen for postpartum depression at your 1-, 2-, 4-, and 6-month well-baby visits using the Edinburgh Postnatal Depression Scale (EPDS). It’s a simple 10-question quiz. If your score is 13 or higher, you likely have PPD. But many providers skip it. Don’t wait for them to ask. If you’re struggling, say it out loud: “I think I might have postpartum depression. Can we talk about treatment options?”
You don’t have to do this alone
There’s no shame in needing help. Taking an antidepressant while breastfeeding isn’t giving up - it’s choosing to be the mom your baby needs. Millions of mothers have done it. Their babies are healthy, thriving, and bonded. You can too. The goal isn’t perfection. It’s connection. And with the right treatment, you can get that back.
Is it safe to breastfeed while taking sertraline?
Yes. Sertraline is the most recommended antidepressant for breastfeeding mothers. Studies show less than 3% of the mother’s dose passes into breast milk, and in over 90% of cases, babies have no detectable levels in their blood. It’s linked to no serious side effects in infants and is considered safe by the CDC, ACOG, and the American Academy of Pediatrics.
Can antidepressants cause my baby to be fussy or have trouble sleeping?
In a small number of cases - about 10-12% of mothers - babies may show mild side effects like increased fussiness, sleep disturbances, or feeding issues. These are usually temporary and resolve with a dose adjustment or by switching medications. Fluoxetine is more likely to cause these effects than sertraline. If you notice changes, track them and talk to your doctor. Most moms find that the benefits of treatment far outweigh these short-term concerns.
Should I pump and dump if I’m on antidepressants?
No, not for most antidepressants. Pumping and dumping is unnecessary for sertraline, paroxetine, or other low-transfer SSRIs. The medication in your milk is too low to harm your baby. The only exception is zuranolone, where current guidelines recommend pumping and discarding milk for one week after the last dose due to limited data. For all other medications, continuing to breastfeed is safer and more beneficial than stopping.
How long does it take for antidepressants to work while breastfeeding?
It typically takes three to four weeks before you notice real improvement in your mood. Some people feel a little better in the first week, but full benefits take time. Don’t stop because you don’t feel better right away. The medication builds up in your system gradually. If you haven’t improved after four weeks, talk to your doctor about adjusting the dose or trying a different medication.
What if my baby has a reaction to the medication?
If your baby shows signs like excessive sleepiness, poor feeding, or unusual crying, contact your pediatrician. Most reactions are mild and can be managed by switching to a different antidepressant - like changing from fluoxetine to sertraline - or adjusting when you take your dose. In rare cases, a blood test may be done to check your baby’s medication levels, but this is rarely needed. The key is not to stop treatment without medical advice - untreated depression is far more dangerous than medication side effects.


Comments
Dr. Marie White
November 1, 2025 AT 20:36I’ve been on sertraline for 8 months while breastfeeding my second. My first kid was super fussy on fluoxetine - couldn’t even nap without screaming. Switching to sertraline was like night and day. Baby slept 6 hours straight for the first time. No side effects, no drama. Just me, my milk, and my sanity.
Doctors need to stop acting like meds are the enemy. The real enemy is pretending you’re fine when you’re not.
Wendy Tharp
November 3, 2025 AT 14:42So you’re just gonna hand out antidepressants like candy now? What about natural remedies? Yoga? Sunlight? Fresh air? My grandma didn’t need SSRIs to raise 5 kids. You’re pathologizing motherhood now. This is why America’s falling apart.
Subham Das
November 4, 2025 AT 21:43One must contemplate the metaphysical weight of maternal pharmacology - is the child’s soul tainted by the chemical imprints of the mother’s despair? Or is healing an act of cosmic reclamation? The body is a vessel, yes, but the milk - oh, the milk - it carries not just nutrients, but the silent screams of a generation taught to swallow their pain. Sertraline, in this light, is not a drug. It is a quiet rebellion against the myth of stoic motherhood. We are not broken. We are simply tired of pretending we are not drowning.
Cori Azbill
November 6, 2025 AT 13:22lol sure, ‘safe’ antidepressants 🤡
Big Pharma’s latest scam. Next they’ll say it’s fine to give your baby Adderall in the bottle. Also, why are we all pretending breastfeeding is some sacred ritual? I formula fed and my kid’s now a Harvard grad. 🤷♀️
Paul Orozco
November 7, 2025 AT 07:24It is imperative to note that the author’s tone, while ostensibly compassionate, subtly promotes pharmaceutical dependency as a primary solution to a condition that may, in many cases, be rooted in systemic social neglect, lack of parental leave, and inadequate community support structures. The suggestion that medication alone is sufficient is, frankly, irresponsible.
Bobby Marshall
November 7, 2025 AT 10:08Man, I wish I’d read this two years ago. I was so lost. Thought I was just ‘bad at momming.’ Took me 5 months to admit I needed help. Sertraline didn’t turn me into a zombie - it turned me back into a person who could hug her kid without crying. My baby’s now 18 months and still nurses like a champ. We’re good. You got this. 💪❤️
Ardith Franklin
November 8, 2025 AT 07:13They never tell you that SSRIs can cause long-term neurological changes in infants. The studies are funded by drug companies. You think they’d let you know if the baby’s brain was rewiring? They’re just waiting for the lawsuits to start. And don’t get me started on zuranolone - it’s a chemical lobotomy disguised as a cure.
Jenny Kohinski
November 9, 2025 AT 00:51I’m from India and my mom took ashwagandha and did yoga after I was born. But honestly? She was also surrounded by family, meals made for her, no pressure to ‘bounce back.’ Here in the US, we’re expected to be supermoms while sleep-deprived and alone. Maybe the real fix isn’t just the pill - it’s the village. 🙏
Aneesh M Joseph
November 10, 2025 AT 18:44fluoxetine bad, sertraline good. whatever. just take zoloft and stop overthinking. my cousin did it. baby fine. mom fine. problem solved.
Deon Mangan
November 11, 2025 AT 04:08Ohhhhh so now we’re supposed to believe Big Pharma’s ‘safe’ labels? 😏
Let me guess - next you’ll say it’s ‘safe’ to give your toddler Adderall in oatmeal. Classic. Also, ‘pump and dump’? Honey, you’re not a cow. But hey, if you wanna spend $200/month on formula because you’re scared of your own medicine, go ahead. 🙄
Vinicha Yustisie Rani
November 11, 2025 AT 21:14In my village, new mothers are wrapped in warm cloths, fed slow-cooked lentils, and held by five women at once. No one asks if they’re ‘depressed.’ They just rest. Here, we give pills and call it care. The medicine helps, yes - but the loneliness? That’s the real illness.
Sharron Heath
November 12, 2025 AT 17:25Thank you for this comprehensive and evidence-based overview. The distinction between medication transfer rates is particularly valuable. I would only add that individual metabolic variation can influence infant exposure - so while population-level data is reassuring, personalized monitoring remains essential. This is exactly the kind of information that should be standard in OB-GYN and pediatric training.
adam hector
November 13, 2025 AT 18:29So let me get this straight - we’ve turned motherhood into a pharmacological experiment? Where’s the moral courage? Where’s the strength in suffering? You don’t need a pill to love your child. You need grit. And maybe a little silence. The modern world has made weakness a diagnosis.
Ravi Singhal
November 14, 2025 AT 06:04sertraline good yeah but did anyone check if baby got any of it in blood? like actual lab test? or just ‘oh its low so its fine’? i think we need more real data not just ‘studies say’
Victoria Arnett
November 15, 2025 AT 00:57I took sertraline and my baby was fine but I cried every day for 3 months before I admitted I needed it