Pediatric Cystic Fibrosis: Essential Care Guide for Children with CF

Pediatric CF Symptom Checker
Select all symptoms that apply to your child:
Symptom Analysis Results
Next Steps:
- If multiple symptoms are present, consider consulting a pediatrician or CF specialist.
- Early diagnosis through sweat test and genetic testing is crucial for effective management.
- Keep a record of symptoms for your healthcare provider.
Quick Takeaways
- CF is a genetic disease that affects lungs, pancreas and growth; early diagnosis saves lives.
- Daily care hinges on airway clearance, nutrition, and targeted medicines.
- A multidisciplinary team-including pulmonologists, dietitians and therapists-keeps the child thriving.
- Parents need a simple routine checklist and an emergency plan for sudden worsening.
- Regular monitoring (sweat test, spirometry, labs) catches complications early.
What Is Pediatric Cystic Fibrosis?
Cystic Fibrosis is a life‑long, autosomal‑recessive disorder caused by mutations in the CFTR gene that disrupt chloride transport across cell membranes. The result is thick, sticky mucus that blocks airways, hampers digestion and fuels chronic infections. In Australia, newborn screening catches most cases before symptoms appear, allowing families to start cystic fibrosis care within weeks of birth.
CF affects roughly 1 in 3,300 newborns in Australia. Kids with CF often experience pancreatic insufficiency, reduced growth, and progressive lung disease if not managed aggressively.
Spotting Early Signs & Diagnosis
Infants may seem healthy at first, but watch for salty‑tasting skin, persistent cough, or poor weight gain. A definitive diagnosis hinges on two tests:
- Sweat Test: measures chloride concentration in sweat; values >60 mmol/L are diagnostic.
- Genetic panel confirming two disease‑causing CFTR gene mutations.
Early detection allows immediate enrollment in specialized CF clinics and initiation of pancreatic enzyme replacement therapy.

Building a Multidisciplinary Care Team
Optimal outcomes rely on coordinated care. Core team members include:
- Pulmonologist - oversees lung health, prescribes inhaled meds.
- Dietitian - designs high‑calorie, high‑fat meals, monitors growth.
- Physiotherapist - teaches airway clearance techniques.
- Social worker, psychologist, and CF nurse coordinator - address mental health, school issues, and logistics.
Regular clinic visits (usually every 1-3 months) keep everyone on the same page.
Core Treatment Pillars
Children with CF need a blend of daily actions and periodic interventions:
- Airway Clearance: removes mucus, reduces infection risk.
- Inhaled Medications: bronchodilators, mucolytics (e.g., dornase alfa), and antibiotics targeting Pseudomonas aeruginosa.
- Pancreatic Enzyme Replacement Therapy (PERT): aids digestion; dosage is weight‑based.
- Nutrition Management: high‑calorie diet, fat‑soluble vitamin supplements (A, D, E, K).
- CFTR Modulators: drugs like ivacaftor, lumacaftor‑ivacaftor that improve CFTR protein function for eligible mutations.
Each pillar interlocks; neglecting one can undermine the others.
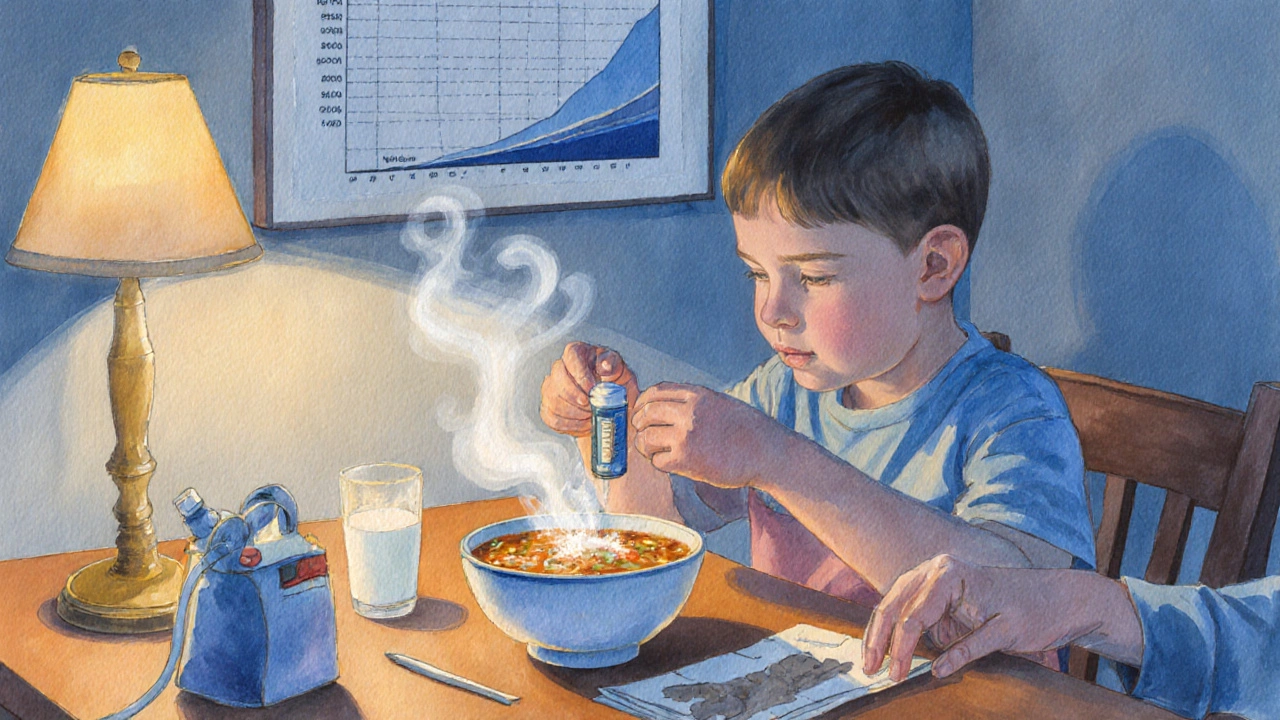
Daily Routine Checklist
Turning treatment into habit helps children feel in control. Below is a sample morning‑evening routine:
- Morning weight check - records growth trends.
- Take prescribed CFTR Modulator with a full glass of water.
- Administer Pancreatic Enzyme Replacement Therapy with breakfast and lunch (dose = lipase units per kg of body weight).
- Perform chosen airway clearance technique (see table below) for 10-15 minutes.
- Inhale prescribed bronchodilator and mucolytic via nebulizer.
- Eat a high‑calorie snack (e.g., avocado toast, cheese toasties) and take vitamin supplements.
- Evening weight check, repeat PERT with dinner, and a second airway clearance session if needed.
Adjust timing based on school schedule and school nurse support; many clinics provide portable nebulizers for school use.
Managing Infections & Hospitalizations
Chronic lung infections are the leading cause of morbidity. Key strategies:
- Routine sputum cultures every 3-6 months to identify pathogens.
- Targeted inhaled antibiotics (e.g., tobramycin) for Pseudomonas colonization.
- Oral antibiotics for early exacerbations, guided by culture sensitivities.
- Monthly spirometry at home using handheld devices; a drop of <10% in FEV1 may signal an upcoming flare.
If symptoms rapidly worsen - fever, increased cough, or chest pain - go to the nearest CF‑experienced emergency department. Early IV antibiotics can prevent longer hospital stays.
Psychosocial Support & School Life
Living with CF isn’t just physical. Children often feel “different” and may face absenteeism. A supportive plan includes:
- Regular counseling sessions to address anxiety or depression.
- Individualized Education Plan (IEP) that accommodates treatment times and physical‑education restrictions.
- Peer support groups - many hospitals run monthly gatherings for kids and parents.
- Family education - teaching siblings how to help with airway clearance without feeling like “caretakers”.
When families understand the why behind each task, children are more likely to cooperate.
Emergency Plan & When to Seek Help
Every household should have a written action plan:
- Identify trusted adult(s) who know the child’s medication list.
- Keep a stocked rescue kit: rescue bronchodilator (albuterol), oral antibiotics, a spare nebulizer kit.
- Red‑flag symptoms - fever >38°C, new chest pain, sudden drop in oxygen saturation (<92%), or vomiting with inability to take enzymes.
- Call the CF clinic’s after‑hours line within 2hours of red‑flag onset; if advised, head to the nearest emergency department.
Practice the plan with the child every 6months so it becomes second nature.
Comparison of Common Airway Clearance Techniques
| Technique | How It Works | Best Age Range | Key Advantages | Potential Drawbacks |
|---|---|---|---|---|
| Chest Physiotherapy (CPT) - percussion | Manual clapping on the back creates vibrations that loosen mucus. | 2months-6years | Low cost, no equipment. | Requires caregiver time; can be uncomfortable. |
| Positive Expiratory Pressure (PEP) devices | Child exhales against resistance, creating back‑pressure to push mucus outward. | 4years-adolescence | Portable, can be self‑administered. | Needs coordination; some children dislike the mouthpiece. |
| High‑Frequency Chest Wall Oscillation (HFCWO) vest | Vibrating vest inflates/deflates rapidly, shaking mucus loose. | 6years-adult | Hands‑free, effective for thick secretions. | Expensive, bulky for school use. |
| Active Cycle of Breathing Technique (ACBT) | Series of controlled breaths, huffs and relaxed exhalations. | 6years-adult | No equipment, teaches self‑management. | Requires learning and practice. |
Frequently Asked Questions
How soon after diagnosis should I start pancreatic enzyme therapy?
As soon as the baby begins feeding. Enzyme doses are calculated by the child’s weight (usually 500-2500lipase units per kilogram per meal) and adjusted based on stool fat content and growth curves.
Can a child with CF live a normal school life?
Yes. With an Individualized Education Plan that allows medication time, a supportive PE teacher, and good infection‑control practices, most kids attend mainstream schools and participate in extracurriculars.
What are the most common infections in pediatric CF?
Early‑life infections often involve Staphylococcus aureus and Haemophilus influenzae. By school age, Pseudomonas aeruginosa becomes dominant, and later Burkholderia cepacia complex can appear in some children.
Are CFTR modulators safe for children under 12?
Recent trials (e.g., for ivacaftor and the triple therapy elexacaftor‑tezacaftor‑ivacaftor) have shown safety in children as young as 6years. Approval varies by mutation type and country, so discuss eligibility with your CF specialist.
How often should my child see a CF clinic?
Typically every 1-3months for stable children, with additional visits after any pulmonary exacerbation or if growth stalls. Telehealth check‑ins can fill gaps between in‑person appointments.


Comments
Sriram K
October 5, 2025 AT 14:03Thanks for sharing this comprehensive guide. As a parent, I find the daily routine checklist especially useful because it turns a complex regimen into a manageable habit. Tracking weight each morning and evening helps catch growth issues early, and the reminder to log symptoms can streamline appointments with the CF team. Keep up the good work and consider adding a printable version for quick reference.
leo calzoni
October 5, 2025 AT 15:13This article pretends to be helpful but it just repeats textbook fluff. Real doctors know better than these generic lists. Stop wasting time.
KaCee Weber
October 5, 2025 AT 16:36Wow, this is such a thorough rundown of pediatric CF care! 😊 I love how you broke down the multidisciplinary team – it really shows how many experts need to coordinate for the best outcomes. The daily checklist is a game‑changer because kids thrive on routine, especially when they can see their progress in a simple weight log. Also, the emphasis on nutrition with high‑calorie meals and vitamin supplements resonates with what many families struggle with. Your section on CFTR modulators is spot‑on, highlighting the newest therapies that are giving hope to many. Keep spreading this valuable info; the community definitely needs more resources like this! 🌟
jess belcher
October 5, 2025 AT 18:00Great guide concise helpful subheadings make it easy to skim for busy parents
Deborah Summerfelt
October 5, 2025 AT 19:23Honestly, all this hype around modulators feels like a marketing ploy – not every kid will qualify and we shouldn't ignore basic airway clearance.
Maud Pauwels
October 5, 2025 AT 20:46Thanks for the effort the layout is clear and the tips are practical I especially appreciate the reminder about vitamin supplements
Scott Richardson
October 5, 2025 AT 22:10Our healthcare system should adopt these protocols nationwide it's time we stop lagging behind other countries.
June Wx
October 5, 2025 AT 23:33This is all just basic stuff.
Justin Atkins
October 6, 2025 AT 00:56The exposition delineates a quintessential framework for managing cystic fibrosis in pediatrics, interweaving clinical rigor with pragmatic daily regimens. By articulating the symbiosis between pulmonary therapies and nutritional optimization, the author crafts a tapestry of care that transcends mere prescription. Moreover, the inclusion of CFTR modulators underscores the evolution of genotype‑directed interventions. Such a comprehensive treatise serves as an indispensable reference for clinicians and caregivers alike.
Laurie Princiotto
October 6, 2025 AT 02:20Meh, looks like a copy‑paste from a pharma brochure 🙄
kristina b
October 6, 2025 AT 03:43In the grand tapestry of pediatric medicine, cystic fibrosis stands as a relentless adversary, demanding both scientific acumen and compassionate stewardship. The guide presented herein embarks upon a noble quest to demystify the labyrinthine regimen that families must navigate daily. It begins with a reverent acknowledgment of the multidisciplinary team, a chorus of specialists whose harmonious collaboration can mitigate the disease's inexorable progression. The pulmonologist, with deft precision, commandeers the airway siege, deploying bronchodilators and mucolytics as artillery against mucus fortifications. Meanwhile, the dietitian orchestrates a caloric symphony, ensuring that each morsel contributes to robust growth amidst malabsorption challenges. The physiotherapist, a silent sentinel, teaches airway clearance techniques that become ritualistic rites of survival. Each pillar, from pancreatic enzyme replacement to vitamin supplementation, is portrayed not as an isolated task but as an interlocking gear in a grand mechanistic design. The daily checklist, rendered with meticulous clarity, transforms chaos into cadence, affording children a semblance of agency over their treatment. The narrative further illuminates the revolutionary promise of CFTR modulators, heralding an era where molecular correction supersedes symptomatic palliation. Yet, the author does not shy away from somber realities; infections remain formidable foes, demanding vigilance through sputum cultures and targeted antibiotics. The emphasis on routine spirometry underscores a proactive ethos, wherein decline is detected before it entrenches. Moreover, the guide wisely counsels families to document symptoms, a practice that empowers both caregivers and clinicians with empirical evidence. In weaving these threads together, the author crafts a mosaic that is simultaneously educational, empathetic, and aspirational. Ultimately, this compendium serves as a beacon, guiding families through the tempestuous seas of cystic fibrosis with steadfast resolve and hope. May each child who follows this protocol experience brighter horizons and a fuller, healthier life.
Ida Sakina
October 6, 2025 AT 05:06It is a moral imperative to prioritize the well‑being of children afflicted with cystic fibrosis. Neglecting comprehensive care betrays our collective responsibility. The guide eloquently underscores the sanctity of vigilant treatment. Let society heed this clarion call.
Amreesh Tyagi
October 6, 2025 AT 06:30Looks thorough but real life is messier than any checklist
Brianna Valido
October 6, 2025 AT 07:53Great point! 😊 Keeping a symptom log really does make appointments smoother. I’ve started using a simple notebook and already feel more organized. Thanks for the reminder!
Caitlin Downing
October 6, 2025 AT 09:16Totally agree life is easier when you write stuff down lol a quick note can save so much stress later on.