Herbal Supplements That Interact with Common Prescription Drugs

More than half of adults in the U.S. take herbal supplements. Many believe these products are harmless because they’re "natural." But what they don’t realize is that some of these supplements can dangerously interfere with prescription medications-sometimes with life-threatening results.
St. John’s Wort: The Silent Medication Killer
St. John’s Wort is one of the most common herbal mood boosters. People use it for mild depression, anxiety, or just to feel better. But here’s the problem: it doesn’t just affect your mood-it affects how your body handles almost every other drug you take.
This herb triggers an enzyme called CYP3A4 in your liver, which speeds up the breakdown of many medications. The result? Your drugs don’t stay in your system long enough to work. For people on cyclosporine after a transplant, this can mean organ rejection. For those on birth control pills, it can lead to unintended pregnancy. In HIV patients taking protease inhibitors, it can cause the virus to rebound.
A 2021 review by the National Center for Complementary and Integrative Health found that St. John’s Wort reduces the blood levels of over 60 prescription drugs by 20% to 80%. One study showed it cut saquinavir (an HIV drug) levels by 51% in just two weeks. And yet, most people never tell their doctor they’re taking it. A 2019 University of Michigan survey found that 76% of supplement users thought "natural" meant "safe." That’s a deadly assumption.
Ginkgo Biloba: The Hidden Bleeding Risk
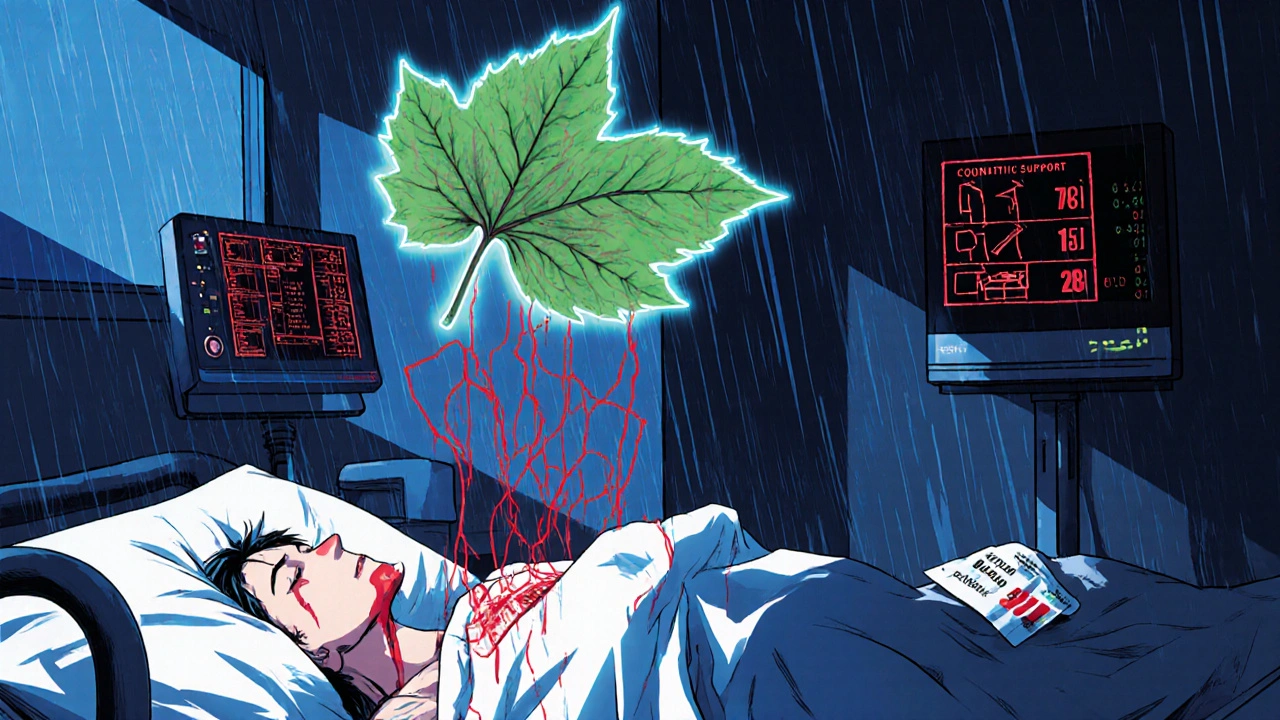
Ginkgo biloba is popular for memory and brain health. It’s in energy drinks, brain supplements, and even some teas. But if you’re on blood thinners like warfarin, apixaban, or aspirin, this herb can turn a minor cut into a medical emergency.
Between 2010 and 2020, the Mayo Clinic documented 23 cases of major bleeding linked to ginkgo and anticoagulants-including three deaths. The herb works by making platelets less sticky, which sounds harmless until you’re on a blood thinner that already does the same thing. Together, they can send your INR (a blood clotting measure) soaring past 8.0. One Reddit user, u/HeartPatient99, described being hospitalized after combining ginkgo with apixaban: "INR spiked to 8.2. I had severe rectal bleeding. My doctor said this happens more than people realize."
Even more troubling? Many supplements labeled "brain support" or "cognitive health" contain ginkgo without listing it clearly. ConsumerLab testing in 2022 found that 73% of these products included ginkgo biloba-often without warning labels.
Garlic: The Unseen Blood Thinner
Garlic is good for your heart. But if you’re taking warfarin or other anticoagulants, your "healthy" garlic supplement could be doing more harm than good. Garlic contains compounds that reduce platelet aggregation, just like aspirin. When taken with blood thinners, it increases bleeding risk.
A 2019 clinical trial at the University of Washington showed garlic supplements reduced the blood levels of saquinavir by 51%. That’s not just a minor drop-it’s enough to make HIV treatment fail. And while some people think eating garlic cloves is safe, supplements are concentrated. One capsule can equal 10 cloves. That’s why the American Academy of Family Physicians classifies garlic as a medium-risk herb for drug interactions.
Coenzyme Q10 and Warfarin: The Hidden Antagonist
CoQ10 is often taken for heart health, energy, or to counteract statin side effects. But it can also interfere with warfarin. Mayo Clinic’s 2022 pharmacokinetic analysis showed CoQ10 reduces warfarin’s anticoagulant effect by 25-30%. That means your INR drops. Your blood clots faster. You’re at risk for stroke or pulmonary embolism.
Unlike St. John’s Wort or ginkgo, this interaction isn’t obvious. You won’t feel it. You won’t bleed. You’ll just wake up one day with a clot. Patients on warfarin who start CoQ10 need weekly INR checks for at least two weeks. Many doctors don’t ask about CoQ10. Patients don’t think to mention it. That’s the gap.
Goldenseal: The Enzyme Blocker
Goldenseal is marketed as an immune booster, especially during cold season. But it’s a powerful inhibitor of CYP3A4-the same enzyme St. John’s Wort activates. Instead of speeding up drug metabolism, goldenseal slows it down. That means drugs build up in your system.
A 2018 study at the University of Toronto found goldenseal reduced the clearance of midazolam (a sedative) by 40%. That’s like doubling the dose. For someone on blood pressure meds, antidepressants, or cholesterol drugs, this can cause toxicity. Symptoms include dizziness, confusion, slow breathing, or even coma. And because goldenseal is often hidden in "immune blends," most people don’t know they’re taking it.
High-Risk Combinations You Should Never Try
- Ginseng + MAO inhibitors: Can trigger serotonin syndrome-high fever, muscle rigidity, seizures.
- Hawthorn + beta-blockers: Can crash your blood pressure below 90/60, leading to fainting or falls.
- Licorice + diuretics: Can drain your potassium to dangerous levels, causing heart rhythm problems.
- Cranberry + warfarin: Controversial, but some studies show INR spikes. Better to avoid unless your doctor confirms it’s safe.

What You Should Do Right Now
Here’s what you need to do if you take any prescription drugs and any herbal supplements:
- List everything you take. Include vitamins, teas, capsules, tinctures-even the ones you only take "once in a while."
- Bring that list to every doctor’s appointment. Don’t wait to be asked. Say it upfront: "I take St. John’s Wort, ginkgo, and garlic pills."
- Ask your pharmacist. Pharmacists are trained to spot these interactions. They have access to databases like Stockley’s and the NCCIH Herb-Drug Interaction Checker.
- Check your labels. Look for ginkgo, St. John’s Wort, garlic, goldenseal, or licorice root. If it’s not listed clearly, don’t take it.
- Watch for warning signs. Unexplained bruising, dizziness, confusion, irregular heartbeat, or sudden changes in mood could mean an interaction is happening.
Why This Problem Keeps Growing
The supplement industry is worth over $62 billion globally. Most products aren’t tested for safety before they hit shelves. The FDA can’t approve them. They can only act after someone gets hurt. In 2022, the FDA issued warnings to 17 companies for hiding actual drugs like statins and antidepressants inside "natural" supplements.
And yet, usage keeps rising. Among adults over 65, nearly 70% take at least one supplement. That’s a huge population on multiple prescriptions. The numbers don’t lie: 1.3 million medication errors happen each year in the U.S. Herb-drug interactions are a major, quiet part of that.
There’s no magic fix. But awareness is the first step. If you’re taking pills for your heart, your blood, your mood, or your thyroid-know what else is in your body. Natural doesn’t mean safe. And silence can kill.
Can I take St. John’s Wort with my antidepressant?
No. St. John’s Wort should never be taken with SSRIs, SNRIs, or other antidepressants. It can cause serotonin syndrome-a potentially fatal condition marked by high fever, muscle rigidity, rapid heartbeat, and confusion. The American Academy of Family Physicians explicitly warns against this combination due to multiple documented cases.
Is ginkgo biloba safe if I’m on blood thinners?
It’s not safe. Ginkgo biloba increases bleeding risk by 300% when combined with warfarin, apixaban, or aspirin. There have been documented cases of major internal bleeding, including fatalities. If you’re on any anticoagulant, avoid ginkgo entirely-even if your doctor says "it’s fine." The evidence is too strong to risk it.
Does garlic interact with prescription drugs?
Yes. Garlic supplements (not food garlic) can reduce the effectiveness of HIV medications like saquinavir by over 50%. They also increase bleeding risk when taken with blood thinners. Even if you’re not on those drugs, garlic can interfere with blood pressure meds and statins. Always check with your pharmacist before taking garlic pills.
What about CoQ10? I take it for statin side effects.
CoQ10 can reduce the effectiveness of warfarin by 25-30%, making your blood clot faster. If you’re on warfarin and start taking CoQ10, your INR could drop dangerously. You’ll need weekly blood tests for at least two weeks. Don’t assume it’s safe just because it’s marketed for heart health.
Are there any herbal supplements that are safe with most medications?
Some have low interaction risk based on current evidence: milk thistle, saw palmetto, black cohosh, and American ginseng. But "low risk" doesn’t mean "no risk." Always disclose everything to your doctor. Even safe herbs can interact unpredictably if you’re on multiple drugs or have liver or kidney issues.
Why don’t doctors know about these interactions?
Most doctors aren’t trained in herbal medicine. Only 25% of supplement users tell their doctors they’re taking them. Plus, only 15% of documented herb-drug interactions have strong clinical trial data. Many are based on case reports. So even when patients speak up, doctors may not have clear guidelines. That’s why you need to be your own advocate.
What should I do if I think I’m having an interaction?
Stop taking the supplement immediately. Call your doctor or go to urgent care. If you’re on warfarin and your INR suddenly spikes or drops, or if you feel dizzy, confused, or have unusual bruising or bleeding, seek help right away. Don’t wait. Herb-drug interactions can turn serious in hours.
What Comes Next
By 2025, major electronic health record systems like Epic will start automatically flagging herb-drug interactions during medication reconciliation. That’s a good step. But it won’t fix the root problem: people still don’t talk about what they’re taking.
The best defense is honesty. Write down every pill, capsule, tea, and tincture you use. Bring it to every appointment. Ask: "Could this interact with what I’m already taking?" If your doctor doesn’t know, ask for a pharmacist consult. Your life might depend on it.


Comments
Nick Naylor
November 20, 2025 AT 20:00St. John’s Wort isn’t just a supplement-it’s a pharmacokinetic wildcard. CYP3A4 induction isn’t theoretical; it’s clinically documented across 60+ drug classes. The FDA doesn’t regulate these products because they’re classified as dietary supplements under DSHEA, which means zero pre-market safety testing. That’s not oversight-it’s regulatory negligence. And don’t get me started on the fact that 76% of users think "natural" equals safe. That’s not ignorance-it’s a public health failure.
Cinkoon Marketing
November 21, 2025 AT 11:28I used to take ginkgo for memory, honestly. Then I read that 2022 ConsumerLab report and realized half the "brain boosters" on my shelf had it hidden under "herbal blend." I stopped everything and just started eating blueberries instead. Still feels like I’m thinking better. Maybe it’s placebo. Or maybe it’s just not poisoning my blood.
Also-why do so many labels say "standardized extract" but never say how much ginkgo biloba is actually in there? That’s not transparency. That’s marketing.
Brianna Groleau
November 22, 2025 AT 08:21I just want to say-I’m 68, on warfarin for AFib, and I’ve been taking CoQ10 for years because my cardiologist said it helps with statin muscle pain. I had no idea it could lower my INR. I just found out last week when my INR dropped from 2.8 to 1.9 in two weeks. I was so scared. I called my pharmacist, and she looked at me like I’d just admitted to drinking bleach. She said, "This happens more than you think."
So now I’m on weekly blood tests. I’m telling every doctor I meet. I’m writing it down. Because I didn’t know. And if I didn’t know, how many others don’t know? We need better labeling. We need better education. We need to stop treating supplements like candy.
Rusty Thomas
November 22, 2025 AT 12:24OMG I JUST REALIZED I’VE BEEN TAKING GOLDENSEAL FOR MY "COLD CURE" FOR THREE YEARS. AND I’M ON LIPITOR AND BLOODY METFORMIN. I’M GOING TO DIE. I’M GOING TO DIIIIIE. MY LIVER IS GOING TO EXPLODE AND MY DOCTOR IS GOING TO SAY "I TOLD YOU SO." I’M CRYING RIGHT NOW. I’M STOPPING IT. I’M GOING TO THE PHARMACY. I’M TELLING EVERYONE. I’M POSTING THIS ON FACEBOOK. I’M TELLING MY CAT. I’M TELLING THE MAILMAN. I’M TELLING THE GROCERY STORE CLERK. I’M TELLING THE GODDAMN CLOWN AT THE FAIR. I’M TELLING EVERYONE.
😭💔
Sarah Swiatek
November 23, 2025 AT 06:49It’s funny how we treat pharmaceuticals like sacred texts-"Doctor prescribed it, so it’s safe"-but when it comes to herbs, we go full New Age mystic and assume they’re harmless because they grow in dirt. The truth? Both are chemicals. Both interact. Both can kill.
The real problem isn’t the supplements. It’s the system that lets them be sold without labeling, without testing, without accountability. And it’s the cultural myth that "natural" equals "good." That’s not science. That’s capitalism dressed up as spirituality.
And yet, the most dangerous thing? The silence. People don’t tell their doctors because they fear judgment. But the doctors? They don’t ask because they’re overworked and undertrained. It’s a perfect storm of neglect. And someone’s going to die because of it. Probably tomorrow. Probably someone you know.
Dave Wooldridge
November 24, 2025 AT 04:48They’re hiding this on purpose. The FDA, Big Pharma, the supplement companies-they’re all in cahoots. Why? Because if people knew how many drugs were being sabotaged by herbs, they’d stop taking the pills. And then the profits would drop. That’s why they let these supplements fly under the radar. That’s why the labels don’t list ginkgo. That’s why CoQ10 is marketed as "heart healthy" while quietly undoing warfarin.
They’re not just selling herbs. They’re selling death. And they’re selling it in pretty little bottles with smiling suns on the label. I’m not paranoid. I’m informed. And I’m not taking another pill until the FDA starts regulating like it’s 1938.
Rebecca Cosenza
November 25, 2025 AT 11:57Stop. Just stop. If you’re on blood thinners and taking anything labeled "natural," you’re playing Russian roulette with your organs. I’m not judging. I’m just saying: you’re not special. Your "holistic lifestyle" won’t save you. Your "clean eating" won’t protect you. Your supplement bottle doesn’t have a soul. It has chemistry. And chemistry doesn’t care about your intentions.
Stop. Talk to your pharmacist. Now.
swatantra kumar
November 25, 2025 AT 13:23Bro, in India we’ve been using turmeric and ashwagandha for 5000 years. You think your fancy FDA knows better? 😎
Also, my uncle took garlic with blood pressure meds and lived to 92. So maybe your science is just... Western bias? 🤷♂️
robert cardy solano
November 26, 2025 AT 18:18My mom took St. John’s Wort for depression after my dad died. She didn’t tell her psych doctor. Three months later, her SSRIs stopped working. She went from feeling okay to suicidal in two weeks. We found out because she accidentally mentioned it during a routine checkup.
She’s fine now. But it took a near-death experience to get her to talk. I just wish someone had told us this before she started.
Pawan Jamwal
November 28, 2025 AT 13:09USA thinks it owns medicine. But we in India know herbs. Ashwagandha, tulsi, neem-these are not "supplements." They’re medicine. Your science is too new to understand. You fear what you don’t control. 🇮🇳💪
Also, your warfarin? It’s synthetic. Our herbs are ancient. Who’s really dangerous?