Bioequivalence Studies: What the FDA Requires Generic Drug Manufacturers to Prove

Why Bioequivalence Matters for Generic Drugs
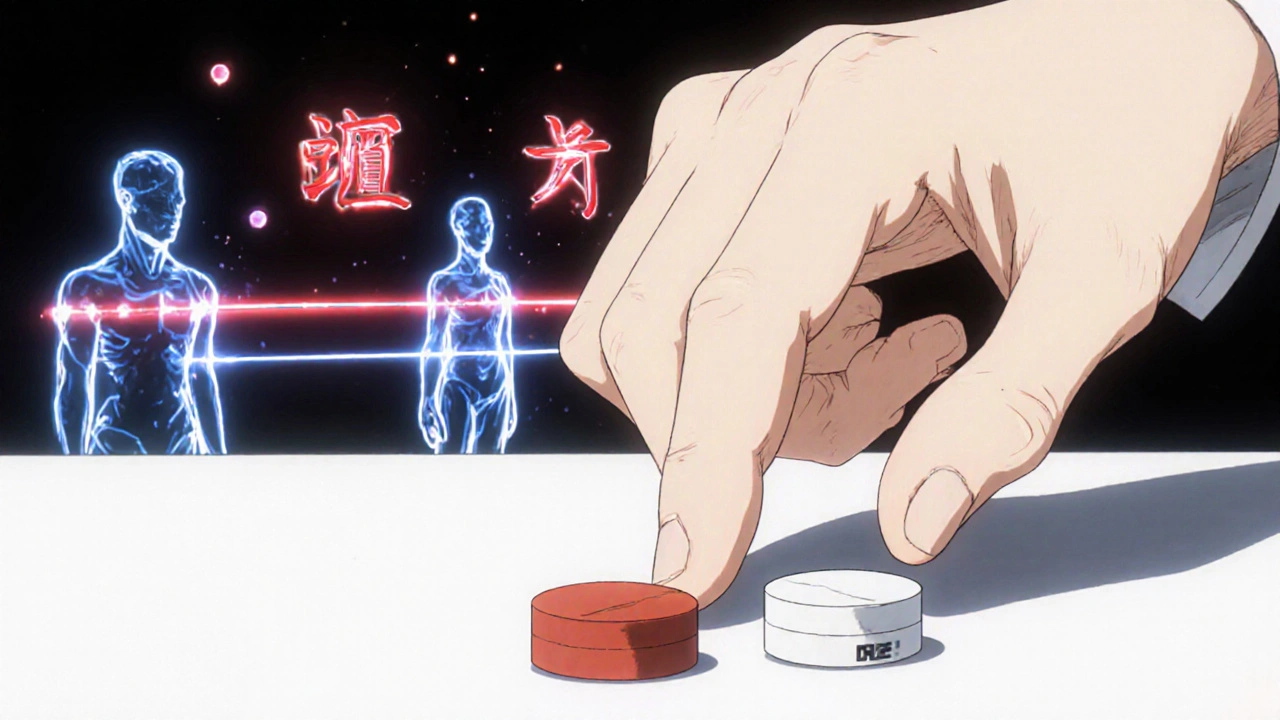
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck-it’s the result of strict testing required by the FDA. Bioequivalence studies are the scientific backbone of generic drug approval. They prove that the generic version delivers the same amount of active ingredient into your bloodstream at the same rate as the original drug. Without this proof, the FDA won’t approve it. This isn’t about cost-cutting-it’s about safety and effectiveness. If a generic drug doesn’t match the brand in how it’s absorbed, it could underdose you-or worse, overdose you. That’s why the FDA treats bioequivalence like a non-negotiable checkpoint.
The Core Rule: 80% to 125%
The FDA’s main standard for bioequivalence is simple but powerful: the 80% to 125% rule. This means that when you compare the generic drug to the brand-name version, the amount of drug that enters your bloodstream (measured as AUC) and how fast it gets there (measured as Cmax) must fall within 80% to 125% of the original. This isn’t a rough estimate-it’s a statistical guarantee. Researchers run studies on 24 to 36 healthy volunteers, take blood samples over time, and use advanced math to calculate the 90% confidence interval. If that interval stays inside 80-125%, the drugs are considered bioequivalent. This rule has been in place since 1992 and hasn’t changed because it works. It’s been validated across thousands of drugs and millions of patients.
How the Studies Are Done
Most bioequivalence studies happen in clinical research units. Volunteers fast overnight, then take either the generic or brand drug. Blood is drawn every 15 to 30 minutes for up to 72 hours. The samples are analyzed using highly sensitive mass spectrometry to measure exact drug concentrations. The study design follows strict rules: crossover design (each volunteer gets both drugs), washout periods between doses, and controlled conditions. Sometimes, the FDA requires a second study under fed conditions-especially if the drug’s absorption changes with food. For example, if a generic antibiotic only works well when taken with a meal, the study must prove it behaves the same way as the brand under those exact conditions. These studies cost between $500,000 and $2 million each, and they’re not easy to get right.
When Bioequivalence Isn’t Tested in People
Not every generic drug needs a human study. The FDA allows biowaivers for certain products where absorption is predictable and doesn’t vary much. This includes eye drops, ear drops, and injectables that are identical in formulation to the brand. For topical creams and gels meant to act on the skin (like hydrocortisone), the FDA may accept lab tests instead. These tests measure how quickly the drug releases from the cream and how well it moves through skin-like membranes. The key is the Q1-Q2-Q3 framework: the generic must have the same active ingredient (Q1), same dosage form and strength (Q2), and similar physical properties like pH and viscosity (Q3). If all three match, the FDA accepts that the drug will behave the same in the body-no volunteers needed. This cuts development time by 6 to 12 months for eligible products.
Special Cases: Narrow Therapeutic Index Drugs
Some drugs are dangerous if the dose is even slightly off. These are called narrow therapeutic index (NTID) drugs. Examples include warfarin, levothyroxine, and phenytoin. For these, the FDA tightens the bioequivalence window from 80-125% to 90-111%. That’s a much smaller range. Why? Because a 10% difference in blood levels could mean a blood clot or a seizure. Manufacturers of NTID generics face extra scrutiny. They must show not just bioequivalence, but consistency across batches. The FDA also requires more data on how the drug behaves in different populations-like older adults or people with liver problems. This is why generic versions of levothyroxine have had recalls and supply issues: even tiny formulation changes can throw off absorption in sensitive patients.
Why So Many Generic Applications Get Rejected
Despite the clear rules, the FDA approves only about 43% of generic drug applications on the first try. Why? Most rejections come down to poor study design. Common mistakes include too few volunteers, poorly timed blood draws, inaccurate lab methods, or incomplete documentation. One company submitted a study where blood samples weren’t stored at the right temperature-invalidating all results. Another used an outdated analytical method that couldn’t detect low drug levels. The FDA’s guidance documents, called Product-Specific Guidances (PSGs), exist to prevent these errors. There are over 2,100 of them, each tailored to a specific drug. Companies that follow these guides have a 68% first-time approval rate. Those who don’t? Just 29%. The message is clear: don’t guess. Follow the guide.

The Future: Modeling and Complex Drugs
The FDA is moving beyond traditional blood tests. For complex drugs like inhalers, injectable gels, or topical patches, the agency now accepts computer modeling. Physiologically Based Pharmacokinetic (PBPK) models simulate how a drug moves through the body based on its chemical properties. These models can replace some human studies, especially for topical products. The FDA has also started using in vitro release testing to predict how a cream or gel will behave in skin. This is a big shift-it means manufacturers can test more prototypes faster and cheaper. But there’s a catch: the models must be validated with real human data first. The FDA isn’t replacing human studies entirely-it’s using science to reduce unnecessary ones. By 2024, draft guidances for 45 complex drug types will be released, including new standards for nasal sprays and transdermal patches.
What This Means for Patients
Every generic drug you take has passed through this exact process. The FDA doesn’t approve generics because they’re cheaper-they approve them because they’ve been proven to work the same. That’s why 90% of prescriptions in the U.S. are filled with generics. They save the healthcare system billions without sacrificing safety. But patients should know: not all generics are created equal in the eyes of the FDA. Some are approved under stricter rules, especially for NTID drugs. If you’re on a drug like levothyroxine and your doctor switches your brand, it’s worth asking if the new generic follows the tighter 90-111% bioequivalence standard. Most do, but not all. The FDA’s transparency helps-its website lists approved generics and the studies they used. You don’t need to be a scientist to understand this: if the FDA says it’s bioequivalent, it means your body will treat it just like the brand.
How Manufacturers Get It Right
Successful generic manufacturers don’t cut corners-they follow the rules. They start by finding the right Reference Listed Drug (RLD) and downloading the FDA’s Product-Specific Guidance for that exact drug. They design their study to match every detail: number of subjects, fasting state, sampling schedule, lab methods. They validate their analytical methods before running the study. They train staff on GLP standards. They document everything. Some even run pilot studies with 6-8 volunteers to catch errors before spending $1 million on the real trial. The FDA’s Domestic Generic Drug Manufacturing Pilot Program rewards companies that source active ingredients and conduct testing in the U.S. These companies get faster reviews. The bottom line? Getting approved isn’t about speed-it’s about precision. One misplaced decimal point in a blood test result can delay approval by a year.






Comments
Lisa Lee
November 22, 2025 AT 09:57U.S. generics are a joke. My cousin in Canada got the same pill, different brand, and had a seizure. FDA doesn't care about real people.
Jennifer Shannon
November 24, 2025 AT 05:38I love how this post breaks it down... it's not just about money, you know? It's about trust. We're talking about people's lives here-heart meds, thyroid pills, seizure drugs-and the fact that the FDA has this 80-125% window, and then tightens it to 90-111% for NTIDs? That's science, not politics. It's beautiful, really. I mean, think about it: a drug that's been tested on 36 people, blood drawn every 15 minutes, mass spec analysis, all to make sure that the $3 pill you buy doesn't kill you... it's almost poetic. And yet, most people just see the price tag and assume it's a scam. But no-it's a miracle of regulatory rigor.
Suzan Wanjiru
November 26, 2025 AT 05:35The biowaiver part is key. For eye drops you don't need humans. The formulation has to match Q1-Q2-Q3. That's the whole thing. Simple. If it's the same active ingredient same concentration same pH same viscosity? It's the same. No need to stick needles in people for every single drop
Kezia Katherine Lewis
November 28, 2025 AT 05:06The Product-Specific Guidance documents are the unsung heroes here. There are over 2,100 of them. Each one is a meticulously crafted roadmap for manufacturers. Without these, the entire system would collapse into chaos. The FDA doesn't just say 'be bioequivalent'-they tell you exactly how to measure it, when to sample, what analytical method to use, even how to handle fasting. It's a masterclass in regulatory precision.
Henrik Stacke
November 28, 2025 AT 18:51I must say, as a Brit who's had to navigate both the NHS and U.S. pharmacy systems, the level of transparency here is astonishing. In the UK, we often get generics without knowing the bioequivalence data-here, you can literally look up the study on the FDA website. It's not just about safety-it's about dignity. Patients deserve to know their medicine has been scrutinized with scientific rigor, not just corporate convenience.
Manjistha Roy
November 28, 2025 AT 23:38The NTID section is critical. Levothyroxine is not like ibuprofen. A 5% difference can mean fatigue or heart palpitations. That's why pharmacists in India also track batch numbers for these drugs. We know what happens when consistency fails. The 90-111% range isn't extra-it's essential. Every patient deserves that precision.
Jennifer Skolney
November 29, 2025 AT 22:21I'm so glad someone finally explained this clearly! 🙌 I was on warfarin last year and my doctor switched my generic and I had to get my INR checked every week for a month. Turns out the new one wasn't under the tighter NTID standard. Now I always check the FDA database before letting them swap. This post saved my life!
Matthew Mahar
November 30, 2025 AT 22:33I think the PBPK modeling thing is huge. I mean, if we can simulate how a drug moves through the body without sticking people with needles, why not? It's faster, cheaper, and less invasive. But I hope they don't skip validation. One time I saw a study where the model was off by 18% because they used the wrong liver enzyme rate. Lesson learned: models need real data to be trusted.
John Mackaill
December 1, 2025 AT 20:27The 43% approval rate makes sense. I've read some of the rejection letters. One company used a centrifuge that spun too fast and degraded the sample. Another didn't record the exact time the volunteer took the pill. It's not about being mean-it's about being exact. One misplaced decimal point, and the whole study's trash. That's science.
Adrian Rios
December 2, 2025 AT 03:46Let me tell you something-this entire system is why I trust American medicine even when I hate the cost. The FDA isn't perfect, but they don't cut corners on this. When I was in med school, we had a case where a generic version of phenytoin caused seizures because the excipients changed the dissolution rate. The FDA responded by tightening the guidance, adding batch-to-batch consistency requirements, and now? It's one of the most rigorously monitored drugs out there. That's not luck. That's accountability.
Casper van Hoof
December 3, 2025 AT 14:40It is an interesting epistemological inquiry to consider the ontological status of bioequivalence as a regulatory construct. One might posit that the 80-125% interval is not a biological truth but a statistical artifact-a consensus boundary imposed by administrative necessity. The human body, after all, is not a controlled laboratory variable. Yet, paradoxically, this artificial threshold has proven empirically sufficient for public health outcomes over three decades.
Richard Wöhrl
December 4, 2025 AT 13:07I want to add something about the fed vs fasted studies. This is huge for drugs like atorvastatin or itraconazole. If the generic only works when taken with food, but the brand was tested fasted? That’s a problem. The FDA requires both. I’ve seen companies skip the fed study to save money-and get rejected. Then they spend another year and $1.2 million redoing it. Don’t be cheap. Do it right the first time.
Pramod Kumar
December 4, 2025 AT 19:29This is the kind of stuff that makes me proud of science. You think generics are just cheap knockoffs? Nah. They’re the quiet heroes of global health. A kid in rural India gets the same levothyroxine as a CEO in Manhattan, because some lab tech in Ohio ran 72 blood draws on 36 volunteers. That’s not capitalism-that’s compassion with a pipette. And the FDA? They’re the referees who make sure no one fakes the game.