TNF Inhibitors and TB Reactivation: Screening and Monitoring Guidelines
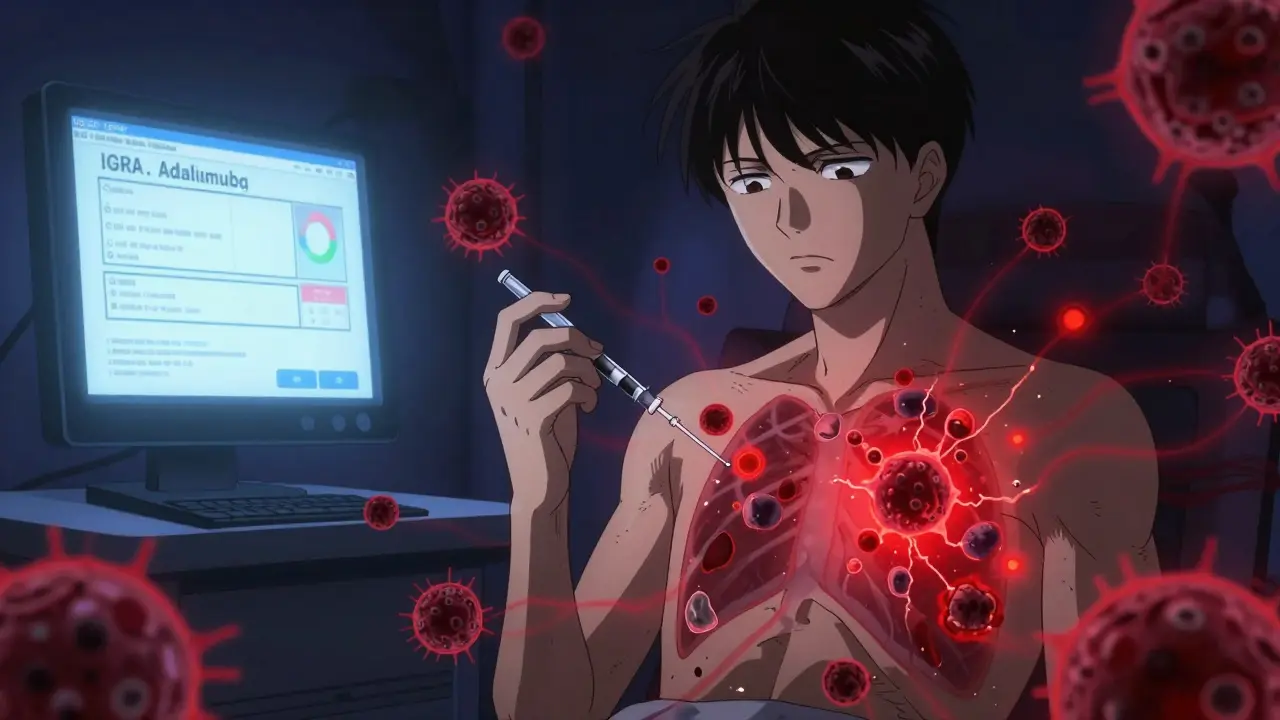
TNF Inhibitor TB Risk Assessment Tool
This tool calculates your risk of TB reactivation when starting TNF inhibitors based on the latest clinical guidelines. Input your specific factors to see your individual risk level.
Key factors considered: Drug type, latent TB treatment status, country of origin, and monitoring timeline.
When you start a TNF inhibitor like adalimumab or infliximab for rheumatoid arthritis, psoriasis, or Crohn’s disease, you’re not just treating inflammation-you’re tipping the balance of your immune system. One of the most serious, yet preventable, risks is tuberculosis (TB) reactivation. This isn’t a rare side effect. It’s a well-documented danger that shows up in about 1 in 100 patients, and it can be deadly if missed.
Here’s the hard truth: TNF-alpha is your body’s natural shield against TB. It holds the bacteria in check inside granulomas-tiny clusters of immune cells that wall off the infection. When you block TNF-alpha with a drug, those walls crumble. The bacteria wake up. And suddenly, a latent infection you never knew you had turns into active, spreading TB.
Not All TNF Inhibitors Are Equal
Not every TNF inhibitor carries the same risk. There’s a clear hierarchy based on how the drug works. Etanercept (Enbrel) is the safest in terms of TB reactivation. It’s a soluble receptor that soaks up free-floating TNF-alpha but doesn’t bind strongly to the version stuck to cell membranes. That’s important-membrane-bound TNF is what keeps granulomas intact.
On the other end are the monoclonal antibodies: infliximab (Remicade) and adalimumab (Humira). These bind tightly to both soluble and membrane-bound TNF. They’re more effective at reducing inflammation, but they also break down granulomas more aggressively. Studies show patients on infliximab or adalimumab are 3 to 4 times more likely to develop TB than those on etanercept. A 2010 British study found the incidence rate ratio was 3.3 for infliximab versus etanercept. A 2024 analysis of 519 patients confirmed adalimumab carried the highest risk-even when patients were treated for latent TB.
Screening Isn’t Optional-It’s Mandatory
Before you even get your first TNF inhibitor shot or infusion, you need two things: a TB test and a full medical history. The American Thoracic Society, CDC, and IDSA all agree: screen everyone. No exceptions.
The two standard tests are the tuberculin skin test (TST) and the interferon-gamma release assay (IGRA). IGRA is more accurate in people who’ve had the BCG vaccine (common outside the U.S.), and it doesn’t need a return visit. But TST is cheaper and widely available. Many clinics use both to be safe. One study found 87% of patients got a TST, 37% got a booster TST, and only 6% got IGRA-meaning most are still being screened with older methods.
But here’s the catch: screening isn’t perfect. About 18% of patients who developed TB after starting TNF inhibitors had negative tests before treatment. Why? Maybe they were infected recently. Maybe their immune system was too weak to react. Maybe the test was done wrong. That’s why guidelines now say: if you’re from a high-TB-burden country-defined as more than 40 cases per 100,000 people per year-you should get treated for latent TB even if your test is negative.
Treating Latent TB Before Starting Therapy
If your test is positive, you need to treat latent TB before starting the biologic. The gold standard has been 9 months of isoniazid. But adherence is a nightmare. About one-third of patients quit because of liver toxicity or just because it’s too long.
Good news: newer regimens are changing the game. In 2024, the FDA approved a 4-month combo of rifampin and isoniazid. Clinical trials showed adherence jumped from 68% to 89%. Another option is 3 months of rifampin alone, or 1 month of rifapentine plus isoniazid. These are faster, safer, and more effective.
Don’t rush. Start TB treatment at least 1 month before your first TNF inhibitor dose. Some experts recommend waiting 2 months, especially if you’re on a high-risk drug like infliximab. Skipping this step is like leaving the door open for TB to walk in.

Monitoring Doesn’t Stop After the First Dose
Screening is step one. Monitoring is step two-and it’s just as critical. Most TB cases happen within the first 3 to 6 months of starting treatment. Half of them show up in the first 90 days.
Every patient on a TNF inhibitor needs to be asked every 3 months: Are you having fevers? Night sweats? Unexplained weight loss? A cough that won’t quit? These aren’t vague symptoms. They’re red flags. And they’re often the only warning you get.
Here’s something many doctors miss: TB on these drugs rarely stays in the lungs. In 78% of cases, it’s extrapulmonary-spreading to the spine, brain, liver, or lymph nodes. That means a normal chest X-ray doesn’t rule it out. You need a high index of suspicion. If a patient on adalimumab comes in with back pain and fatigue, don’t just call it arthritis flaring. Think TB.
What Happens When TB Does Reactivate?
If TB shows up, you stop the TNF inhibitor immediately. Start standard anti-TB therapy-isoniazid, rifampin, pyrazinamide, ethambutol-for at least 6 months. But here’s the twist: sometimes, when you start TB treatment, the immune system overreacts. That’s called TB-IRIS-immune reconstitution inflammatory syndrome.
It happens in about 13% of patients. Symptoms flare up 45 days after starting TB drugs, often after the last TNF inhibitor dose. Fever spikes. Swollen lymph nodes. Painful joints. It can look worse than the original infection. Treatment? Steroids. Often high doses-60 mg of prednisone daily-for months. It’s a delicate balance: treat the TB without letting the immune system go haywire.
And the mortality rate? Higher than regular TB. Anti-TNF-associated TB has a 23% higher death rate. Why? Because it’s often missed, diagnosed late, or mistaken for a flare of the original autoimmune disease.

The Real-World Challenges
Even with clear guidelines, things go wrong. In one survey, 27% of patients had delays in starting TNF inhibitors because their LTBI treatment wasn’t properly documented. Others had negative tests but still got TB. One rheumatology nurse on Reddit shared a case: a patient from India had a negative TST, started adalimumab, and developed disseminated TB in 3 months. Repeat tests were still negative.
In low-resource settings, 80% of clinics can’t even access IGRA. They rely on TST, which gives false positives in BCG-vaccinated patients. That leads to unnecessary treatment-or worse, missed cases.
And cost? Screening adds $150-$300 per patient. But it’s pennies compared to hospitalization, surgery for spinal TB, or a funeral.
The Future: Safer Drugs on the Horizon
Researchers aren’t just accepting this risk. They’re trying to fix it. New drugs are in development that target TNF-alpha without touching the membrane-bound version. Early animal studies show these selective inhibitors cut TB reactivation risk by 80% compared to current drugs. Phase II trials are underway. If they work, we could have a new generation of biologics that control inflammation without leaving patients vulnerable to TB.
Until then, the rules are simple: test before you treat. Treat latent TB. Monitor closely. Don’t assume a negative test means safety. Don’t delay treatment because of paperwork. And never forget: the same drug that gives someone back their mobility can also kill them-if you don’t watch for TB.






Comments
Anu radha
December 17, 2025 AT 21:08This made me so nervous-I’m from India and my aunt just started Humira last month. I didn’t know TB could come back like this. Please, if you’re taking these drugs, get tested. Even if you feel fine.
Jigar shah
December 18, 2025 AT 16:54Interesting breakdown of TNF inhibitor risk stratification. The membrane-bound vs. soluble TNF distinction is clinically significant but often overlooked in primary care. Etanercept’s lower risk profile is well-supported by meta-analyses, particularly in BCG-vaccinated populations.
Sachin Bhorde
December 19, 2025 AT 19:52Y’all need to stop skipping the LTBI treatment just cuz it’s annoying. I’m a nurse in Mumbai and we’ve had 3 cases this year where folks started biologics without finishing isoniazid. One guy ended up with spinal TB. Bro, it’s not worth it. 4-month rifampin combo? Do it. Your spine will thank you. 🙏
Jane Wei
December 21, 2025 AT 02:12So… basically we’re trading mobility for a 1% chance of dying from something we didn’t even know we had? Cool. Cool cool cool.
Meghan O'Shaughnessy
December 21, 2025 AT 12:33In India, TB is everywhere. My cousin had latent TB and never knew until she got sick after starting a biologic. The clinic didn’t even offer IGRA-just a TST, which was negative. She spent 6 months in the hospital. This isn’t theoretical. It’s real life.
Radhika M
December 23, 2025 AT 01:20My mom is on adalimumab. We did the IGRA and TST together. Positive. Started 4-month rifampin. Took 2 weeks to get the meds because of insurance. Now she’s waiting 2 more weeks before her first shot. Everyone should just get it done-no excuses.
Anna Giakoumakatou
December 24, 2025 AT 19:10How quaint. We’ve replaced natural immunity with pharmaceutical convenience, and now we’re surprised when the immune system throws a tantrum? We’ve outsourced our biology to Big Pharma and now we’re surprised when the system crashes. The irony is delicious.
Erik J
December 26, 2025 AT 15:55Is there any data on whether TB reactivation rates differ between rural vs urban patients in high-burden countries? I’m curious if access to diagnostics affects outcomes beyond just test type.
Virginia Seitz
December 28, 2025 AT 03:01Just got my IGRA back-negative! 😌 Took 3 days. Got my Humira shot today. Fingers crossed. 🤞
Peter Ronai
December 28, 2025 AT 03:37Of course the CDC says screen everyone. But what about the 18% who test negative and still get TB? That’s not screening-that’s gambling with lives. And you want to trust a $150 test to keep someone from dying? Pathetic.
Victoria Rogers
December 28, 2025 AT 14:06Why are we letting Indian patients get biologics when their country can’t even test properly? This isn’t global health-it’s American arrogance with a side of TB. We should ban TNF inhibitors for non-US citizens until they fix their infrastructure.
BETH VON KAUFFMANN
December 29, 2025 AT 19:52Let’s be real-the 4-month rifampin regimen is the future. Adherence jumped from 68% to 89%? That’s not just better, that’s revolutionary. We’ve been clinging to 9 months of isoniazid like it’s a sacred text. Time to update the playbook. Also, extrapulmonary TB on biologics is terrifying because it looks like a flare. I’ve seen it. It’s not arthritis. It’s TB. And it kills.
And yes, the mortality rate is 23% higher. That’s not a side effect. That’s a systemic failure in triage and suspicion. Every rheumatologist should be trained to ask: ‘Is this a flare-or is this TB?’ before prescribing another dose.
And don’t get me started on how many patients get cleared because they’re ‘low risk’-except they’re from Bangladesh, Nigeria, or Peru. Screening isn’t optional. It’s a moral obligation. If you’re not doing IGRA + TST + risk assessment, you’re not practicing medicine. You’re guessing.
And the new selective TNF inhibitors? If they work, they’ll be the biggest breakthrough in biologics since the first anti-TNF. No more granuloma demolition. Just inflammation control. That’s the future we need.
Until then? Test. Treat. Wait. Monitor. Don’t be lazy. Don’t assume. Don’t skip the 3-month check-ins. Because one missed night sweat could be the last thing you ever hear from your patient.
amanda s
December 31, 2025 AT 00:00So you’re telling me my 78-year-old dad, who’s been on Humira for 3 years, could’ve had TB this whole time and we didn’t know? That’s medical malpractice. I’m suing the hospital. This is a lawsuit waiting to happen.