Brand-Name Medications: What They Are, Why They Matter, and How They Compare to Generics
When you hear brand-name medications, original prescription drugs developed and marketed by pharmaceutical companies under a patent. Also known as originator drugs, these are the first versions of a medicine to hit the market after years of research and clinical testing. They’re the ones you see advertised on TV, prescribed by your doctor, and often covered by insurance with a higher copay. But why do they still exist when cheaper generics are everywhere? The answer isn’t just about profit—it’s about trust, consistency, and sometimes, real differences in how your body responds.
Generic drugs, lower-cost versions of brand-name medications that contain the same active ingredient. Also known as follow-on drugs, they must meet strict FDA standards to prove they work the same way in your body. But proving bioequivalence doesn’t always mean they feel the same. Some patients report different side effects, absorption rates, or even effectiveness when switching from a brand-name drug like Daxid (sertraline) to its generic version. That’s not because generics are bad—it’s because inactive ingredients, manufacturing processes, and even the shape of the pill can change how your body handles the medicine. For people with sensitive conditions like epilepsy, depression, or HIV, those tiny differences matter.
That’s why FDA approval, the official process that evaluates whether a drug is safe and effective for public use. Also known as drug clearance, it’s the baseline every medication—brand or generic—must pass before it’s sold. The FDA doesn’t just look at the active ingredient. They check how the drug is made, where it’s made, and whether the manufacturing plant follows cGMP rules. That’s why some brand-name drugs still hold an edge: they’ve been around longer, their production has been fine-tuned over decades, and their quality control is more predictable. Meanwhile, generic drug recalls have risen in recent years due to overseas manufacturing issues, making some patients stick with the original—even at a higher price.
And it’s not just about safety. When you’re managing chronic conditions like OCD, depression, or HIV, switching from a trusted brand-name drug like Clofranil or Combivir to a generic can feel risky. You’ve already found what works. Why mess with it? Your pharmacist might say they’re the same. But if you’ve had a bad reaction or your symptoms changed after switching, you’re not imagining it. That’s why many doctors still write prescriptions with "dispense as written"—because they know what’s worked for you.
Brand-name medications aren’t just about marketing. They’re about reliability. For some people, that’s worth paying more for. For others, generics are perfectly fine. The key is knowing the difference—and knowing when to ask your doctor or pharmacist if a switch is truly safe for you.
Below, you’ll find detailed comparisons between brand-name drugs and their alternatives—from ED treatments like Vidalista Black and Kamagra Effervescent to antidepressants, eye drops, and HIV meds. You’ll see what’s changed over time, what still holds up, and what you should ask before making any switch.
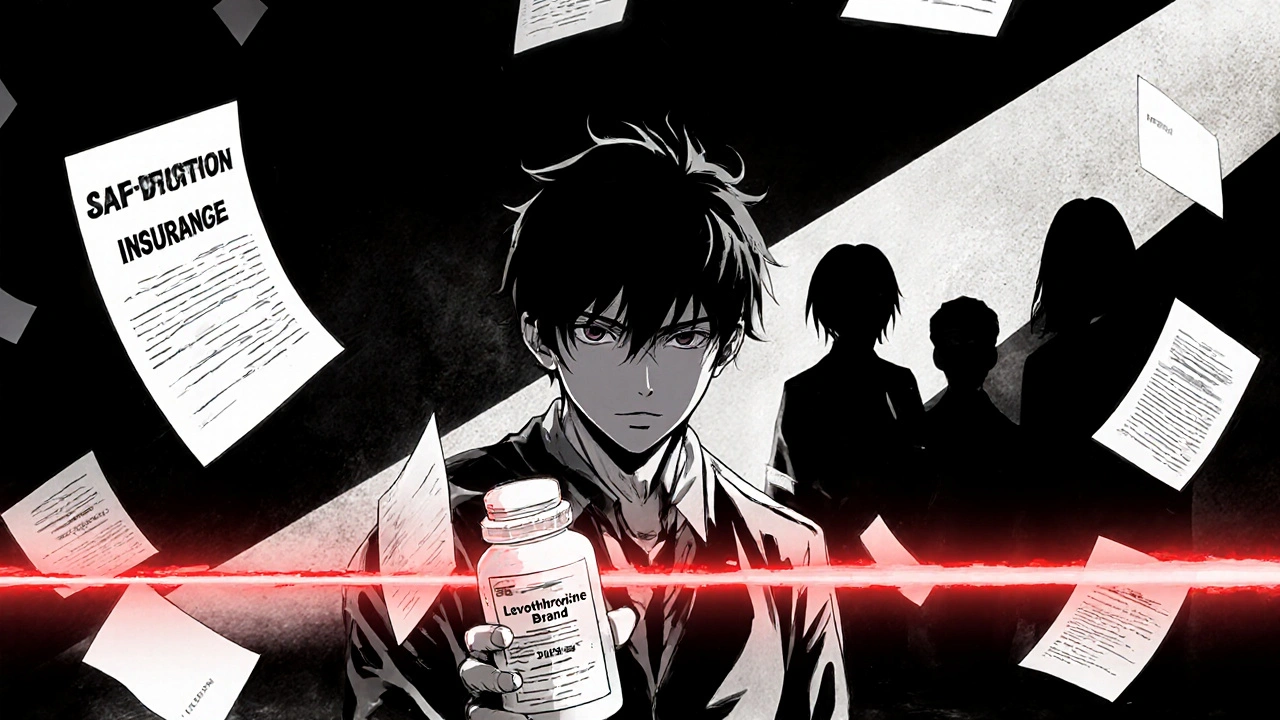
Prior Authorization for NTI Drugs: When Insurers Require Brand-Name Medications
NTI drugs like levothyroxine and phenytoin require extreme dosing consistency. Yet insurers often force patients to jump through hoops for brand-name versions. Learn why this happens, how it risks health, and what you can do about it.