Opioids: Understanding the Risks of Tolerance, Dependence, and Overdose
When you take an opioid for pain-whether it’s oxycodone after surgery or morphine for cancer-you’re not just getting relief. You’re also setting off a chain reaction in your brain that can lead to tolerance, dependence, and in the worst cases, overdose. These aren’t rare side effects. They’re predictable outcomes of how these drugs work. And understanding them isn’t just medical knowledge-it’s life-saving information.
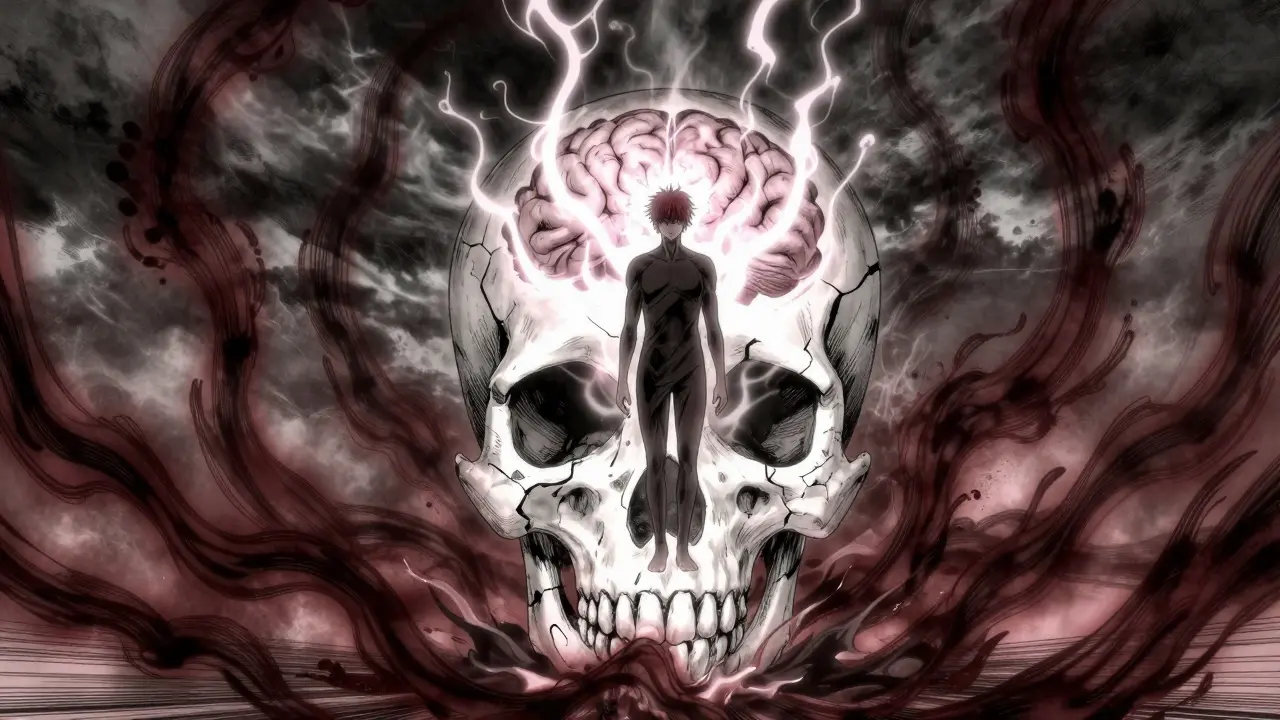
How Opioids Work (And Why They’re So Dangerous)
Opioids bind to mu-opioid receptors in your brain, spinal cord, and gut. This blocks pain signals and floods your reward system with dopamine. That’s why they work so well for pain-and why they feel so good. But that same mechanism is what makes them risky.
Every time you take an opioid, your brain adapts. Receptors become less responsive. Your body starts producing fewer natural painkillers. Over time, you need more of the drug to get the same effect. That’s tolerance. It doesn’t mean you’re addicted. It means your biology has changed.
But here’s the trap: tolerance to pain relief and euphoria develops faster than tolerance to respiratory depression-the one effect that can kill you. That’s why someone who’s been using opioids for months can still overdose if they take a little more than usual. Their body has learned to ignore the high, but not the slow breathing.
Tolerance: The Silent Escalation
Tolerance isn’t a sign of weakness. It’s a biological fact. Studies show that within six months of regular opioid use, most patients need 25-50% higher doses to get the same pain control. That’s not because the pain got worse. It’s because the receptors have dulled.
This isn’t just a problem for people using opioids recreationally. It happens to patients too. A 2019 study found that 32% of people prescribed opioids for chronic pain started misusing them within a year-not because they wanted to get high, but because the original dose stopped working.
And the brain doesn’t just adapt to pain relief. It also rewires itself to crave the drug. Neuroinflammation kicks in. Glutamate signaling increases. The brain starts associating cues-like a pill bottle, a certain time of day, or even a smell-with the drug’s effect. That’s how tolerance turns into dependence.
Dependence: When Your Body Demands the Drug
Dependence means your body needs the drug to function normally. Stop taking it, and you don’t just feel bad-you get sick. Withdrawal symptoms include nausea, vomiting, muscle aches, anxiety, insomnia, and sweating. It’s not fun. But it’s not usually life-threatening.
What makes dependence dangerous is the fear of withdrawal. People keep using not because they love the high, but because they can’t stand the crash. That’s why so many people stay on opioids long after their injury has healed.
And here’s something many don’t realize: dependence can happen even when you take opioids exactly as prescribed. There’s no magic threshold. It can occur after just a few weeks. That’s why guidelines now recommend opioids for acute pain only for 3-7 days, and never as a first-line treatment for chronic pain.

Overdose: The Deadly Gap
An opioid overdose happens when breathing slows to a stop. The brain stops telling your lungs to breathe. You turn blue. You lose consciousness. Without help, you die.
But overdose isn’t just about taking too much at once. It’s about timing, tolerance, and the drug you’re using.
Fentanyl is 50-100 times stronger than morphine. A few milligrams can kill. And because it’s often mixed into heroin or counterfeit pills without the user’s knowledge, people think they’re taking a normal dose-and die.
Heroin and methadone are also major players in overdose deaths. But here’s the twist: people who’ve been clean for weeks or months are at the highest risk. Why? Because their tolerance has dropped. Their body no longer expects the drug. If they relapse and take their old dose, their system can’t handle it.
Research shows 65% of opioid overdose deaths happen in people who’ve had prior treatment. One Reddit user wrote: “After 6 months clean, I used my old dose and nearly died-paramedics said I was clinically dead for 4 minutes.” That’s not an outlier. It’s the rule.
Why Some Opioids Are Safer Than Others
Not all opioids are created equal. Buprenorphine, for example, is a partial agonist. It activates opioid receptors, but only up to a point. After a certain dose, it stops increasing the effect. That’s called a ceiling effect. It means even if you take more, you won’t get more high-and you won’t stop breathing as easily.
That’s why buprenorphine is used in Medication-Assisted Treatment (MAT). It reduces cravings and withdrawal without the same overdose risk as full agonists like oxycodone or fentanyl.
Meanwhile, fentanyl has become the deadliest opioid in the U.S. In 2021, it was involved in 70.3% of all opioid overdose deaths. That’s up from just 19.5% in 2015. Illicit fentanyl is now found in fake pills that look like oxycodone, Xanax, or Adderall. People think they’re taking something else-and they don’t survive.

The Hidden Risk: Lost Tolerance After Treatment
Recovery is hard. But the biggest danger doesn’t come during treatment-it comes after.
When someone stops using opioids, their body slowly resets. Receptors return to normal. Tolerance fades. That’s good. But if they relapse, even with a small dose, their body is unprepared. They’ve lost their buffer.
Harm reduction groups like Narcan Saves Lives report that 87% of overdose reversals since 2018 involved people who had been clean for at least a week. That’s not random. It’s predictable. And it’s why naloxone (Narcan) is now handed out freely in pharmacies, clinics, and even libraries.
Naloxone reverses an overdose in minutes. It’s safe. It doesn’t get you high. It doesn’t work on other drugs. But if someone’s overdosing on opioids, it can bring them back to life. That’s why every person in recovery, their family, and even friends should carry it.
What’s Changing Now
There’s been progress. In 2023, the U.S. passed the Mainstreaming Addiction Treatment (MAT) Act. It removed the old “X-waiver” that only allowed 150,000 doctors to prescribe buprenorphine. Now, all 1.1 million licensed physicians can. That’s a game-changer.
Prescription rates have dropped by nearly half since 2012. But the gap hasn’t been filled with safer alternatives-it’s been filled with fentanyl. The DEA seized 1,200% more fentanyl between 2015 and 2022.
The FDA now requires opioid manufacturers to fund education on tolerance and overdose risk. And the NIH has poured $1.5 billion into research for non-addictive pain treatments. One promising direction? Biased ligands-drugs that block pain without triggering respiratory depression.
But the most powerful tool right now is access. MAT with buprenorphine or methadone cuts overdose risk by half. Naloxone distribution has reduced fatal overdoses by 34% in communities that use it widely.
What You Need to Do
If you’re prescribed opioids:
- Ask if there’s a non-opioid option first.
- Use the lowest dose for the shortest time possible.
- Never mix with alcohol, benzodiazepines, or sleep aids. That combination kills.
- Get a naloxone kit. Keep it in your wallet, your car, your bathroom.
- Talk to your doctor if you feel you need more pills to get the same relief. That’s tolerance. It’s not failure. It’s biology.
If you or someone you know is in recovery:
- Never use alone. Always have someone nearby who knows how to use naloxone.
- Start low if you relapse-even if you used to take 10 pills a day, your body can’t handle it now.
- Connect with MAT programs. Buprenorphine isn’t “replacing one drug with another.” It’s giving your brain time to heal.
- Carry naloxone. Always.
If you’re a friend or family member:
- Don’t judge. Shame doesn’t stop addiction. Knowledge does.
- Learn how to use naloxone. It takes 30 seconds to learn.
- Keep the kit charged and accessible. Don’t hide it in a drawer.
- Encourage treatment-not punishment.
Opioids are not evil. They’re tools. Powerful, dangerous tools. Used right, they save lives. Used wrong, they end them. The difference isn’t willpower. It’s understanding.
Can you become dependent on opioids even if you take them exactly as prescribed?
Yes. Physical dependence can develop after just a few weeks of regular use, even when following a doctor’s instructions exactly. This is a biological response to the drug, not a sign of addiction. Dependence means your body has adapted and will experience withdrawal if the drug is stopped abruptly. Addiction involves compulsive use despite harm, which is different from dependence.
Why are people who’ve been clean at higher risk of overdose than new users?
After stopping opioid use, your body loses tolerance. Your brain and lungs no longer expect the drug. If you relapse and take the same dose you used before, your system can’t handle it. Your breathing can stop. This is why 65% of opioid overdose deaths occur in people with prior treatment history. It’s not about how much you used-it’s about how much your body can tolerate now.
Is fentanyl more dangerous than other opioids?
Yes. Fentanyl is 50 to 100 times more potent than morphine. A dose as small as 2 milligrams can be fatal. It’s often mixed into counterfeit pills that look like oxycodone or Xanax, so users don’t know they’re taking it. In 2021, fentanyl was involved in 70% of all opioid overdose deaths in the U.S. It’s not just stronger-it’s unpredictable and invisible.
Does naloxone work on all drug overdoses?
No. Naloxone only reverses overdoses caused by opioids like heroin, fentanyl, oxycodone, or morphine. It has no effect on overdoses from alcohol, cocaine, benzodiazepines, or methamphetamine. But if someone is unconscious and not breathing, and you suspect opioids are involved, give naloxone anyway. It’s safe and won’t harm someone who didn’t take opioids.
Is buprenorphine just replacing one addiction with another?
No. Buprenorphine is a medication used to treat opioid use disorder, not to replace one addiction with another. It reduces cravings and withdrawal without causing euphoria or respiratory depression at standard doses. It allows people to stabilize, rebuild their lives, and eventually reduce or stop use-with support. Studies show it cuts overdose risk by 50%. It’s medicine, not substitution.
Can you overdose on opioids even if you’ve used them for years?
Yes. Tolerance to euphoria and pain relief develops faster than tolerance to respiratory depression. Long-term users may feel fine taking a high dose, but their breathing can still shut down. Mixing opioids with alcohol, sleep aids, or benzodiazepines increases this risk dramatically. Even experienced users are not immune to overdose.
If you’re using opioids, know your risks. If you’re helping someone in recovery, know how to save their life. Tolerance, dependence, and overdose aren’t abstract medical terms. They’re real, preventable dangers-and the tools to fight them are already here.






Comments
Joie Cregin
January 18, 2026 AT 08:29Man, I wish my doc had told me this before I got hooked on oxycodone after my knee surgery. I thought tolerance meant I was weak-turns out my brain just got smart. Now I carry Narcan in my purse like my lipstick. No shame in that.
Christina Bilotti
January 18, 2026 AT 12:07Oh wow. A whole essay on how biology works. Did you also write a 10-page paper on how gravity pulls things down? Groundbreaking. I’m sure everyone reading this was just sitting around wondering why their lungs stopped breathing after a dose.
brooke wright
January 19, 2026 AT 04:04My cousin died last year from a fake Xanax laced with fentanyl. She was 24. She just wanted to sleep. I keep thinking if someone had handed her a Narcan kit at the party, she’d be here. Why isn’t this in every pharmacy? Why isn’t it taught in high school?
Nick Cole
January 19, 2026 AT 07:51Let me cut through the noise: if you’re prescribed opioids, you’re already in the danger zone. Not because you’re weak, but because the system is rigged. Doctors get paid to write scripts, not to explain neuroadaptation. I’ve seen too many people go from ‘just for the pain’ to ‘just to feel normal.’ This post? It’s the truth wrapped in a warning label. Listen to it.
Riya Katyal
January 19, 2026 AT 17:38Oh so now we’re blaming the drugs? How original. People have been doing stuff they shouldn’t since cavemen. Maybe the real issue is that we’ve turned every human problem into a medical one. Just say no, ladies. And stop acting like your brain is a broken toaster.
waneta rozwan
January 21, 2026 AT 06:00DO YOU KNOW WHAT HAPPENS WHEN YOU STOP TAKING OPIATES? YOUR BODY BECOMES A NIGHTMARE. I WENT THROUGH WITHDRAWAL IN A MOTEL ROOM WITH NO WATER AND A BABY CRYING. I THOUGHT I WAS DYING. I WASN’T. BUT I WISHED I WAS. THIS ISN’T A STORY. THIS IS A WAR. AND WE’RE LOSING.
Nicholas Gabriel
January 22, 2026 AT 17:30Let me just say-this is the most important thing I’ve read all year. I’m a nurse. I’ve seen it. I’ve held people as they stopped breathing. I’ve handed Narcan to moms who didn’t know how to use it. Please-don’t wait until it’s too late. Get the kit. Learn the steps. Teach your kids. Keep it in your glove compartment. Your neighbor might need it tomorrow. And if you’re in recovery? You’re not broken-you’re brave. And you deserve support, not stigma.
Cheryl Griffith
January 22, 2026 AT 20:07I was on opioids for three months after my back surgery. I didn’t even realize I was dependent until I tried to stop. The sweats, the shakes, the panic-it felt like my bones were crawling out of my skin. I didn’t want to get high. I just didn’t want to feel like death. I’m now on buprenorphine and honestly? It’s the first time in two years I’ve slept through the night. This isn’t about replacing one thing with another. It’s about giving your brain a chance to heal.
swarnima singh
January 23, 2026 AT 10:45its not the drugs its the void inside… we all crave escape… opioids just give u a mirror to see how empty u really are… i know… i’ve been there… the pain was never in my spine… it was in my soul… and no pill can fix that… only love… or maybe just silence…
Kasey Summerer
January 25, 2026 AT 02:49So fentanyl’s the new devil? Cool. Next you’ll tell me meth is just sugar water. 😏 I’ve seen a guy OD on a fake Percocet in a parking lot. Dude was holding a Starbucks cup. Didn’t even know he was holding death. Narcan saved him. Now he’s in a MAT program. Life’s weird like that. 🤷♂️
john Mccoskey
January 25, 2026 AT 18:41Let’s be brutally honest: the entire opioid narrative is a carefully constructed myth designed to shift blame away from the pharmaceutical industry and onto the individual. Tolerance? Of course it develops-your body adapts to any pharmacological insult. Dependence? It’s an inevitable physiological consequence of receptor modulation, not a moral failing. Overdose? It’s a direct result of unregulated potency and the criminalization of drug use, which prevents safe consumption environments. The fact that we’re still treating addiction as a behavioral issue rather than a public health crisis speaks volumes about our collective failure. The MAT Act is a start, but without decriminalization, safe supply, and housing support, we’re just rearranging deck chairs on the Titanic. And don’t get me started on how naloxone is treated like a Band-Aid on a hemorrhage. It’s not a solution-it’s triage. We need systemic change, not pamphlets and pity.