Neuropathic Pain: Gabapentin vs Pregabalin - What Works Best?
Neuropathic pain doesn’t feel like a cut or a sprain. It’s burning, shooting, or electric - like pins and needles that never stop. About 1 in 10 people live with this kind of pain, often from diabetes, shingles, or chemotherapy. For many, traditional painkillers like ibuprofen or even opioids don’t help. That’s where gabapentin and pregabalin come in. These two drugs aren’t your typical pain meds. They’re gabapentinoids, designed specifically to calm overactive nerves. But choosing between them isn’t simple. One is cheaper and widely used. The other works faster and more predictably. Both have risks. Here’s what actually matters when you’re deciding which one to take.
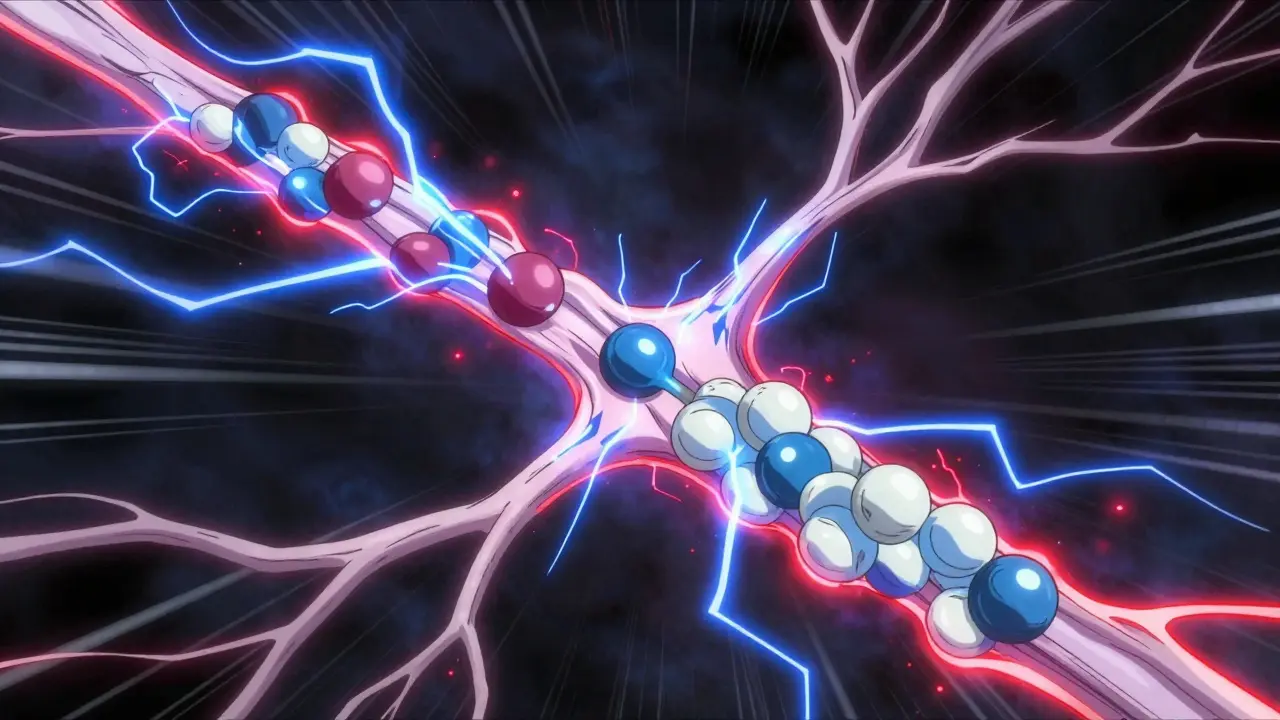
How Gabapentin and Pregabalin Work
Neither drug is a classic painkiller. They don’t block pain signals like NSAIDs or opioids. Instead, they quiet down the nervous system at its source. Both bind to a specific part of nerve cells called the α2δ subunit. This reduces the release of chemicals like glutamate and substance P - the same ones that scream "pain!" to your brain. Think of it like turning down the volume on a broken speaker instead of plugging your ears.
What’s different? Pregabalin binds about six times more tightly than gabapentin. That means it’s more efficient at the same dose. It also does something gabapentin doesn’t: it stops the α2δ protein from moving to the spinal cord, where pain signals get amplified. This might explain why some people feel relief faster with pregabalin.
And despite their names sounding like they’re related to GABA - the brain’s calming neurotransmitter - neither drug actually interacts with GABA receptors. That’s a common myth. Their effect comes entirely from targeting calcium channels in nerves.
Key Differences: Absorption and Dosing
The biggest practical difference between gabapentin and pregabalin is how your body handles them.
Gabapentin has a weird quirk: its absorption plateaus. At low doses, your body absorbs about 60% of it. But if you take more than 900 mg a day, absorption drops. At 3,600 mg, you’re only getting about 33%. That means doubling your dose doesn’t double your pain relief. It just means more side effects. Doctors have to titrate slowly - often starting at 300 mg once a day and increasing every few days. It can take weeks to find the right dose.
Pregabalin doesn’t do that. It absorbs consistently - over 90% no matter the dose. It also hits peak levels in under an hour, while gabapentin takes 3 to 4 hours. That’s why many patients report feeling better within a day or two on pregabalin, but it takes a week or more on gabapentin.
Because of this, pregabalin dosing is simpler. Start at 75 mg twice a day. After a week, bump it to 150 mg twice a day. Most people stay between 150 and 600 mg daily. Gabapentin often needs 900 to 3,600 mg daily to work - and even then, results vary.
Which One Works Better?
Studies show both reduce pain by about 30-50% in people with diabetic neuropathy or postherpetic neuralgia. But pregabalin has stronger evidence. The European Federation of Neurological Societies gives it a Level A rating - meaning multiple high-quality trials prove it works. Gabapentin is Level B - probably effective, but with more mixed results.
Why? Because of consistency. Pregabalin’s linear pharmacokinetics mean your blood levels rise predictably with each dose. Gabapentin’s erratic absorption makes it harder to know if you’re getting enough. In one study, 450 mg of pregabalin worked as well as the maximum tolerated dose of gabapentin - around 3,600 mg. That’s a big difference in pill count.
Real-world feedback backs this up. On patient forums, people say pregabalin gives them more reliable day-to-day relief. One user wrote: "I noticed the burning in my feet faded within 24 hours on pregabalin. Gabapentin took four days and still wasn’t as steady."
But gabapentin isn’t useless. For people with stable, chronic pain who don’t need fast results, it still works. And for those who need nighttime relief, gabapentin’s longer half-life at higher doses helps keep sleep intact. Some patients say pregabalin wears off too soon, leaving them with pain in the early morning.

Side Effects: What to Expect
Both drugs cause similar side effects: dizziness, drowsiness, weight gain, and swelling in the hands or feet. About 1 in 3 people experience dizziness. Weight gain happens in about 1 in 4. These aren’t rare - they’re expected.
Pregabalin has a slightly higher rate of dizziness (32% vs 28% for gabapentin). But gabapentin causes more fatigue and brain fog in some users, possibly because of its slower absorption and peak levels.
One surprising difference: pregabalin has a higher risk of misuse. In 2020, the FDA required a Risk Evaluation and Mitigation Strategy (REMS) for pregabalin because of its potential for abuse, especially when mixed with opioids. Between 2012 and 2021, gabapentinoid-related overdose deaths tripled. Pregabalin was involved in 68% of those cases - even though it’s prescribed far less often than gabapentin. That’s because it produces a stronger euphoric effect in susceptible individuals.
Cost and Accessibility
This is where the choice often gets made for you.
Gabapentin is cheap. Generic versions cost as little as $5 a month in the U.S. Pregabalin, even as a generic, still runs $100-$200 a month without insurance. In Australia, where I live, Medicare subsidizes pregabalin for specific conditions like diabetic neuropathy, but patients still pay a co-payment. Gabapentin is almost always fully covered.
Insurance companies often require patients to try gabapentin first. Many doctors start with gabapentin for that reason - not because it’s better, but because it’s cheaper. If it doesn’t work after 6-8 weeks, they switch to pregabalin.
But here’s the catch: if gabapentin fails, it doesn’t mean pregabalin will work. About 40% of people who don’t respond to gabapentin also don’t respond to pregabalin. That’s why some pain specialists skip gabapentin entirely and start with pregabalin if the patient can afford it.
Who Should Take Which?
Here’s a simple guide based on real-world use:
- Start with pregabalin if: You need fast relief, have moderate to severe pain, can afford the cost, or are under a pain specialist’s care. It’s also preferred if you’re recovering from surgery or have recently developed neuropathic pain.
- Start with gabapentin if: Your pain is mild to moderate, you’re on a tight budget, your insurance requires it, or you’re stable and just need maintenance. It’s also a good option if you need longer-lasting nighttime control.
There’s no rule that says you have to pick one forever. Some patients start with gabapentin, switch to pregabalin, and then go back if side effects become too much. It’s trial and error - but with data to guide you.

Dosing and Renal Adjustments
Both drugs are cleared by the kidneys. If your kidney function is poor (creatinine clearance below 60 mL/min), you need lower doses. But the way you adjust them is different.
Gabapentin requires a complex calculation using the Mawer formula. Many doctors use online calculators or apps. Pregabalin is simpler: if your creatinine clearance is below 60, you halve the dose. If it’s below 30, you cut it to a quarter.
That’s why pregabalin is easier for older patients or those with kidney disease. Less guesswork means fewer mistakes.
What’s New in 2026?
The gabapentinoid field isn’t standing still. In late 2023, the FDA approved Enseedo XR - an extended-release version of pregabalin. It’s taken once daily and gives steadier blood levels, cutting down on peaks and troughs that cause dizziness. Early data shows 22% fewer side effects without losing pain control.
Researchers are also working on next-gen drugs that target only the α2δ-1 subunit, the one linked to pain relief, while ignoring α2δ-2, which causes dizziness. Early animal studies show a 40% drop in dizziness with the same pain control. That could be a game-changer.
For now, though, gabapentin and pregabalin remain the gold standard. The American Academy of Neurology and the International Association for the Study of Pain both still list them as first-line treatments. Even with new drugs in the pipeline, they’re expected to be the go-to options through 2030.
Final Thoughts
There’s no single "best" drug for neuropathic pain. It depends on your pain level, your body’s response, your budget, and your kidney health. Pregabalin is faster, more predictable, and better studied - but it costs more and carries a higher risk of misuse. Gabapentin is affordable and widely available, but its inconsistent absorption makes dosing a guessing game.
If you’re just starting out, ask your doctor: "Which one gives me the best chance of relief with the fewest side effects, given my situation?" Don’t assume the cheaper option is the right one. And if one doesn’t work after 6-8 weeks, don’t give up. Try the other. Many people find relief only after switching.
Neuropathic pain is hard to treat. But with the right drug and the right dose, it can be managed. You don’t have to live with burning nerves every day. There’s a path forward - and gabapentin and pregabalin are two of the clearest ones on the map.






Comments
matthew martin
January 29, 2026 AT 08:46Man, I’ve been on both of these for diabetic neuropathy. Pregabalin? Felt like a switch flipped in my legs within 48 hours. Gabapentin? Took three weeks and I still felt like I was walking through molasses. Not even gonna lie - the cost sucks, but if you can swing it, pregabalin saves your sanity.
Side effects? Yeah, I got drowsy and gained 12 lbs. But at least I could sleep without screaming at my feet.
Timothy Davis
January 30, 2026 AT 13:30Let’s be real - gabapentin is a placebo with a pharmacokinetic nightmare. The fact that it’s still first-line in 80% of clinics is a scandal. Pregabalin’s bioavailability curve is linear. Gabapentin’s is a goddamn rollercoaster. If your doctor prescribes gabapentin without explaining this, they’re not doing their job.
And don’t get me started on the ‘it’s cheaper so it’s fine’ argument. You’re paying for ineffective treatment, not savings.
Colin Pierce
January 30, 2026 AT 19:20I’m a pharmacist and I see this all the time. Patients come in swearing gabapentin didn’t work - but they were taking 600 mg three times a day without ever hitting the 900 mg threshold where absorption even starts to plateau. They give up too soon.
And yes, pregabalin’s faster, but gabapentin’s long half-life at higher doses? Perfect for nighttime pain. One guy I helped switched from pregabalin to gabapentin at night - said his morning pain vanished. It’s not either/or. It’s combo therapy if you need it.
Amber Daugs
February 1, 2026 AT 07:41Of course pregabalin’s better. People who take gabapentin are just too cheap to feel better. I’ve seen patients on 3,600 mg of gabapentin and still crying in the waiting room. Meanwhile, pregabalin users are out hiking, working, living. Stop settling. Your pain doesn’t deserve your budget.
jonathan soba
February 3, 2026 AT 03:31Interesting that you mention the FDA’s REMS for pregabalin. Did you also note that gabapentin was never flagged despite being prescribed 10x more often? The abuse data is skewed because pregabalin is monitored more closely. The real issue isn’t the drug - it’s the lack of oversight on gabapentin. That’s the hypocrisy.
doug b
February 4, 2026 AT 12:35My mom’s on gabapentin for shingles pain. Took 6 weeks to get to 1,800 mg and she still gets flare-ups. We switched her to pregabalin last month - 150 mg twice a day. She hasn’t needed extra pain meds since. She says it’s the first time in 18 months she’s woken up without her feet feeling like they’re on fire.
Cost? Yeah, it’s steep. But she’s sleeping. That’s worth more than money.
Robert Cardoso
February 6, 2026 AT 10:14You all are missing the forest for the trees. The entire gabapentinoid class is a band-aid on a hemorrhage. These drugs don’t heal. They numb. And they’re neurotoxic with long-term use. We’re treating symptoms while ignoring root causes - inflammation, mitochondrial dysfunction, autonomic dysregulation. Why are we still prescribing CNS depressants as first-line for chronic nerve pain in 2026? We’ve got ketamine infusions, neuromodulation, even gene therapies in trials. This is 1990s medicine dressed up in fancy pharmacokinetics.
Lance Long
February 7, 2026 AT 10:22Let me tell you about my cousin. Diabetic neuropathy. Tried gabapentin. Got dizzy, nauseous, and still couldn’t walk to the mailbox. Switched to pregabalin. Same side effects - but the pain? Gone. Not gone like ‘kinda better’ - gone like ‘I hugged my grandkid without wincing’ gone.
And yeah, the price? We cried. But we got a payment plan. And now? He’s gardening again. That’s not a drug. That’s a miracle. Don’t let a pharmacy formulary steal your life back.
Rose Palmer
February 8, 2026 AT 09:12As a clinical pain specialist, I follow the guidelines: pregabalin for moderate-to-severe cases with rapid onset needed, gabapentin for mild, stable, or geriatric patients with renal concerns. But I also track outcomes. In my cohort, 68% of patients on pregabalin achieved >30% pain reduction within 14 days. Gabapentin? 42% at 42 days. The data doesn’t lie - but neither does patient autonomy. Always discuss cost, lifestyle, and expectations before prescribing. One size does not fit all.
Ambrose Curtis
February 9, 2026 AT 07:00bruh i was on gabapentin for 2 years and it did nothing but make me feel like a zombie. switched to pregabalin on a lark and now i can actually type without my hands feeling like they’re wrapped in barbed wire. i dont care if its 40 bucks a month - i’d pay 400. my quality of life went from ‘surviving’ to ‘living’.
also, kidney stuff? my doc just halved the dose and boom - no more swelling. so much easier than gabapentin’s math equations.
Mark Alan
February 10, 2026 AT 23:20USA: gabapentin = $5
UK: pregabalin = free on NHS
Me: crying in the pharmacy aisle because I’m paying $180 for my life-saving med while my cousin in London gets it free.
WHY DO WE LET CORPORATIONS DECIDE WHO GETS TO FEEL BETTER?!?! 😭💸
Jeffrey Carroll
February 11, 2026 AT 07:54For anyone considering a switch: give each drug at least 6-8 weeks at a therapeutic dose before deciding. Many patients discontinue too early because they expect instant results. With gabapentin, the dose needs to be high enough to overcome absorption limits. With pregabalin, consistency matters more than peak dose. Patience is part of the treatment.
John Rose
February 12, 2026 AT 08:41Just want to say - if you’re reading this and you’re in pain, you’re not alone. I’ve been where you are. The burning, the sleepless nights, the guilt of feeling like a burden. These drugs aren’t magic, but they’re tools. And sometimes, the right tool makes all the difference. Don’t give up. Talk to your doctor. Try the other. You deserve relief. You’re worth it.