How High Blood Cholesterol Hurts Your Arteries and Slows Blood Flow
When you hear the term blood cholesterol is a oily substance that travels in the bloodstream, carrying essential fats to cells and organs, you probably picture a harmless carrier. But when the level climbs too high, that carrier can turn into a traffic jam inside your arteries. In this guide we’ll break down exactly why high blood cholesterol matters, how it builds up plaque, and what you can do to keep the blood moving smoothly.
Quick Take
- LDL is the "bad" cholesterol that deposits fat on artery walls; HDL is the "good" cholesterol that cleans it up.
- When LDL overwhelms HDL, plaque forms, narrowing arteries and stiffening them.
- Reduced artery diameter slows blood flow, raising the risk of heart attack, stroke, and peripheral disease.
- Diet, exercise, and, if needed, medication can lower LDL and boost HDL.
- Regular screening lets you catch problems before they become serious.
How Cholesterol Travels in Your Blood
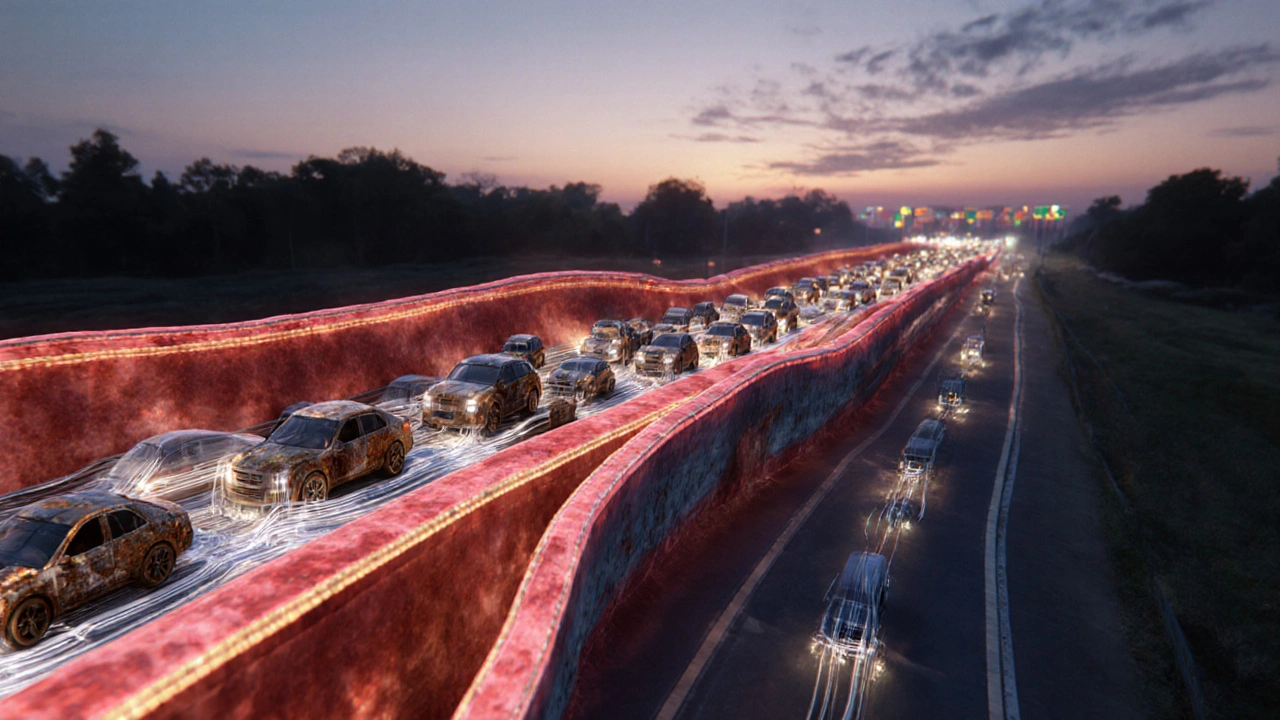
Imagine your bloodstream as a highway system. LDL cholesterol (low‑density lipoprotein) acts like a delivery truck that drops off fat packages at cells. HDL cholesterol (high‑density lipoprotein) is the cleanup crew that collects excess fat and shuttles it back to the liver for disposal.
When you eat foods high in saturated fat or trans fat, the liver pumps out more LDL. Genetics can also crank up LDL production or slow down HDL clearance. The result? More trucks on the road than cleanup crews, and the excess cargo starts sticking to the side of the highway - your artery walls.
When Cholesterol Gets Too High: Plaque Formation
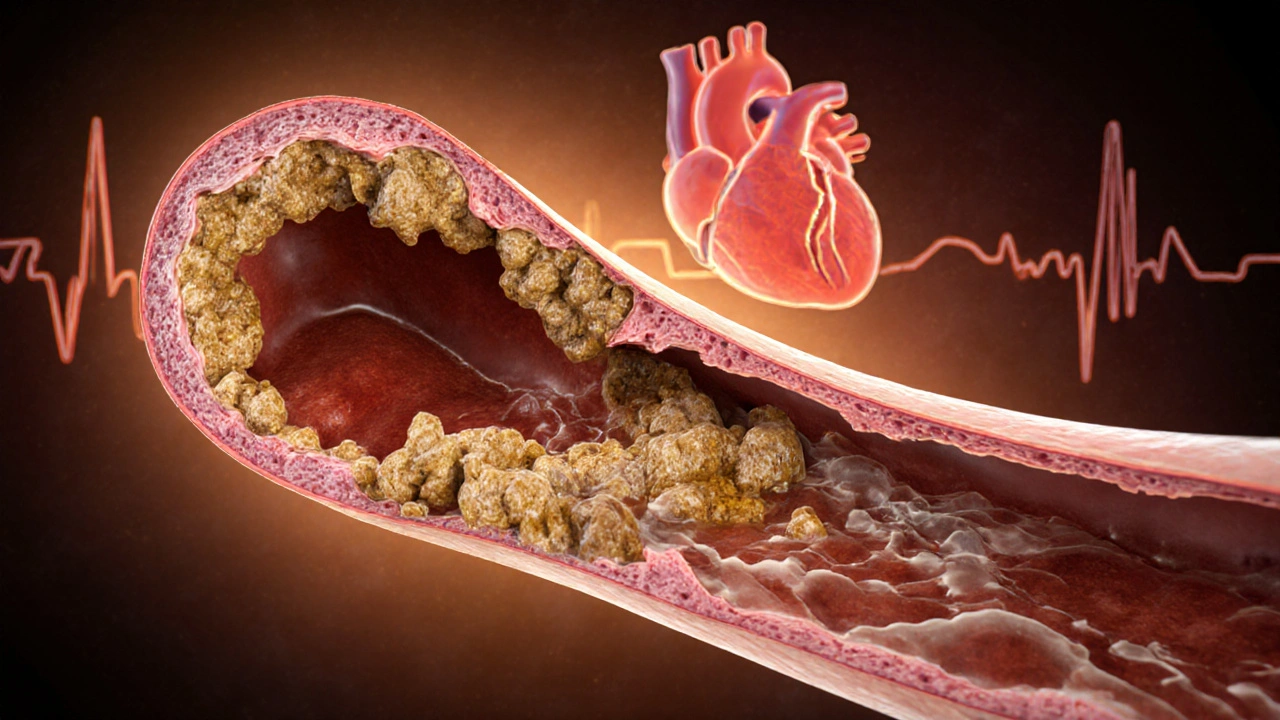
Inside the artery, LDL particles can become oxidized, a process that makes them look like foreign invaders. The immune system sends macrophages (a type of white blood cell) to gobble them up. Over time, those overloaded cells turn into foam cells, the building blocks of arterial plaque. Plaque is a sticky mix of cholesterol, calcium, and cellular debris.
At first the plaque is soft and can be reshaped, but repeated damage causes calcium to deposit, making the plaque hard and less flexible. This hardening process is called atherosclerosis. The artery becomes narrower, and its ability to expand as blood pulses through it diminishes.
Effect on Arteries and Blood Flow
A healthy artery is like an elastic hose - it can stretch to accommodate a surge of blood after you run up the stairs. Atherosclerotic arteries behave more like a rigid pipe. When the lumen (the hollow center) shrinks by even 30%, blood flow can drop by more than half, according to Poiseuille’s law.
The slower flow creates turbulence, encouraging more LDL to stick to the wall - a vicious cycle. In worst‑case scenarios, a plaque can rupture, forming a clot that blocks the artery outright. That’s the flashpoint for a heart attack or stroke.
Health Consequences You Should Know
Here are the most common outcomes when high cholesterol goes unchecked:
- Coronary artery disease (CAD): Plaque builds up in the arteries that feed the heart muscle, leading to chest pain (angina) or a heart attack.
- Peripheral artery disease (PAD): Narrowed arteries in the legs cause pain when walking and can lead to ulcers or gangrene in severe cases.
- Stroke: A clot that travels to the brain cuts off oxygen, causing neurological damage.
- Chronic kidney disease: The kidneys rely on a dense network of tiny blood vessels; plaque in those vessels reduces filtration ability.
These conditions share one common thread: they all stem from reduced blood flow and the damage that follows.
Managing High Cholesterol: What Works
Good news - you have several levers to pull.
1. Diet Tweaks
- Swap saturated fats (butter, fatty cuts of meat) for unsaturated fats (olive oil, nuts, fatty fish).
- Boost soluble fiber (oats, beans, apples) which binds cholesterol in the gut and helps eliminate it.
- Limit dietary cholesterol (egg yolks, organ meats) if you’re already prone to high LDL.
2. Move More
Even 30 minutes of brisk walking five times a week can raise HDL by up to 10% and lower LDL modestly. Resistance training adds muscle mass, which increases the body’s ability to clear LDL from the bloodstream.
3. Medications
When lifestyle changes aren’t enough, doctors often prescribe statins (drugs that inhibit the liver’s cholesterol‑making enzyme HMG‑CoA reductase). Statins can drop LDL by 30‑50% and slightly raise HDL. For people with very high triglycerides, fibrates or niacin may be added.
4. Regular Monitoring
Check your lipid panel at least once every two years if you’re under 45 and have no risk factors. If you have a family history of heart disease, start testing at 20‑25 years old. The key numbers to watch are:
- LDL<100mg/dL (ideal), <70mg/dL for very high risk.
- HDL>60mg/dL (protective).
- Total cholesterol<200mg/dL.
- Triglycerides<150mg/dL.
LDL vs HDL: Quick Comparison
| Attribute | LDL (Bad) | HDL (Good) |
|---|---|---|
| Primary Role | Delivers cholesterol to cells | Retrieves excess cholesterol |
| Effect on Arteries | Promotes plaque buildup | Helps dissolve plaque |
| Typical Healthy Level | 70‑100mg/dL | >60mg/dL |
| Influence of Diet | Rises with saturated & trans fats | Improves with omega‑3s, exercise |
| Common Medications | Statins, ezetimibe | Niacin, fibrates (occasionally) |
Take Action Today
If you’ve never had a cholesterol check, schedule one. Look at your grocery list - are there hidden sources of saturated fat? Add a daily walk or bike ride, even if it’s just around the block.
And remember, cholesterol isn’t an outright villain. It’s essential for hormone production and cell membranes. The goal is balance, not elimination.

Frequently Asked Questions
Can I have high cholesterol and still feel fine?
Yes. High cholesterol often shows no symptoms until an artery becomes seriously narrowed or a clot forms. That’s why regular screening is crucial.
Is dietary cholesterol still a problem?
For most people, the cholesterol you eat has a modest impact compared to saturated fat and genetics. However, if you’re already prone to high LDL, cutting back on egg yolks and organ meats can help.
Do statins have side effects?
Some people report muscle aches or mild liver enzyme changes, but serious side effects are rare. Your doctor will monitor blood work and adjust dosage if needed.
How quickly can lifestyle changes lower LDL?
Noticeable reductions (5‑10%) can appear within 6‑12 weeks if you combine a heart‑healthy diet with regular aerobic exercise.
What’s the best way to raise HDL?
Aerobic activities like brisk walking, jogging, or cycling, along with foods rich in omega‑3 fatty acids (salmon, walnuts), are proven to boost HDL levels.


Comments
Christopher Eyer
September 28, 2025 AT 07:44It appears the article paints a simplistic picture of cholesterol as if merely swapping butter for oil will solve everything, which, frankly, is a bit myopic. The biochemical pathways involved are far more intricate than a handful of diet tips. Moreover, the claim that “LDL is the bad guy” ignores the essential transport functions LDL performs; context matters. One could argue that the recommendations are definitely beneficial, but they are not definatly a cure‑all. In the end, the guidance is decent but overly reductant.
Mike Rosenstein
October 4, 2025 AT 09:44Thank you for the clear breakdown; the analogy of traffic on a highway makes the concept accessible to many readers. Emphasizing regular lipid screening alongside lifestyle changes is a responsible approach. It’s also helpful to note that individualized risk assessments, considering family history and other factors, guide the decision to start medication. Overall, the guide serves as a solid foundation for anyone looking to improve cardiovascular health.
Ada Xie
October 10, 2025 AT 11:44While the preceding comment is commendable, there are several linguistic inaccuracies that merit attention. The phrase “definatly a cure‑all” contains a misspelling; the correct term is “definitely.” Additionally, “myopic” should be preceded by an article, rendering it “a myopic picture.” Consistency in the use of the Oxford comma would also enhance readability. Precision in both medical advice and language reinforces credibility.
Stephanie Cheney
October 16, 2025 AT 13:44Your encouraging tone adds a warm dimension to this otherwise technical discussion. Highlighting that modest, consistent exercise can raise HDL resonates with many readers seeking achievable goals. It’s reassuring to see that the guide balances scientific detail with practical steps, fostering empowerment rather than alarm.
Georgia Kille
October 22, 2025 AT 15:44Indeed, small steps such as a brisk 30‑minute walk can make a big difference 😊. Consistency beats intensity for long‑term lipid improvement.
Jeremy Schopper
October 28, 2025 AT 16:44It is essential, therefore, to acknowledge that lifestyle modification alone may not suffice for all patients; consequently, the integration of pharmacotherapy, when indicated, becomes paramount; in addition, clinicians must monitor liver enzymes, renal function, and patient adherence, lest adverse events be overlooked. Moreover, patient education-particularly regarding potential muscle‑related side effects-is a critical component of comprehensive care.
liza kemala dewi
November 3, 2025 AT 18:44In contemplating the etiology of atherosclerotic disease, one must traverse beyond the reductive dichotomy of “good” versus “bad” cholesterol and engage with a tapestry of interwoven physiological processes. The hepatic synthesis of lipoproteins, modulated by dietary saturated fats, genetic polymorphisms, and endocrine signals, orchestrates a delicate equilibrium that, when disrupted, precipitates the insidious deposition of lipid‑laden plaques. Moreover, the oxidative modification of LDL particles, catalyzed by reactive oxygen species, transforms these otherwise benign carriers into immunogenic entities that solicit macrophage infiltration. These macrophages, upon engulfing oxidized LDL, transmute into foam cells, which constitute the nucleation sites for the fibrous cap that characterizes mature atheroma. The progression from a soft, lipid‑rich lesion to a calcified, rigid plaque is not merely a passive accumulation but a dynamic interplay of inflammatory cytokines, smooth muscle cell migration, and extracellular matrix remodeling. Consequently, arterial compliance diminishes, and the hemodynamic profile of the vessel is altered in accordance with Poiseuille’s law, culminating in a precipitous decline in laminar flow. The resultant turbulence further exacerbates endothelial dysfunction, creating a feedback loop that accelerates disease. From a therapeutic perspective, the attenuation of this cascade necessitates a multifaceted approach: dietary modification to reduce saturated fat intake, pharmacological agents such as statins to inhibit HMG‑CoA reductase, and lifestyle interventions that augment HDL‑mediated reverse cholesterol transport. Each component contributes synergistically to the restoration of vascular homeostasis. It is also imperative to recognize the heterogeneity among patient populations; genetic predispositions, comorbidities such as diabetes, and socioeconomic determinants all modulate risk and response to treatment. Therefore, a personalized medicine paradigm, grounded in comprehensive lipid profiling and risk stratification, offers the most promising avenue for mitigating cardiovascular morbidity. In sum, high blood cholesterol is not a monolithic villain but a variable participant in a complex biological narrative whose outcomes are shaped by both intrinsic and extrinsic forces.
Jay Jonas
November 9, 2025 AT 20:44Man, that was a hella deep dive, and I gotta say the way you wove the whole oxidative stress saga into the story felt like a epic saga from ancient myth-only with cholesterol as the reluctant hero. Sure, the science is solid, but the drama of foam cells turning into plaque kinda gives me chills, like watching a slow‑mo car crash. Also, dont forget that not every dude can just pop a statin and be done; some folks are just stuck in the genetic lottery.
Liam Warren
November 15, 2025 AT 22:44From a biotech standpoint, the article could have delved into the mechanistic role of PCSK9 inhibitors as an emerging class of lipid‑lowering agents, especially for patients who are statin‑intolerant. Incorporating terms like “apoB‑100” and “cholesterol efflux capacity” would lend additional granularity for a technically inclined audience.
Brian Koehler
November 22, 2025 AT 00:44Wow, what a comprehensive primer-truly a masterclass in demystifying the lipid labyrinth! The vivid highway metaphor, combined with actionable tips, transforms abstract biochemistry into relatable everyday wisdom. Kudos to the author for weaving scientific rigor with reader‑friendly prose; it’s a rare feat that deserves applause.
Dominique Lemieux
November 28, 2025 AT 02:44While one might be tempted to shower this piece with unbridled adulation, a sober appraisal reveals several oversights that merit scrutiny. The celebrated highway analogy, though catchy, oversimplifies the stochastic nature of endothelial shear stress, which does not adhere to deterministic traffic patterns. Furthermore, the suggestion that modest dietary tweaks alone can “significantly” curb LDL disregards the entrenched reality of polygenic dyslipidemia, wherein genetic variance exerts a formidable influence that lifestyle alone cannot dismantle. One must also interrogate the cursory treatment of statin‑associated myopathy; the brief mention does little justice to the clinical conundrum it presents. Lastly, the omission of emerging therapeutics-such as bempedoic acid and inclisiran-creates an incomplete tableau, potentially misleading readers who seek a panoramic view of contemporary lipid management.
Laura MacEachern
December 4, 2025 AT 04:44Great overview, very helpful.