Fiber Supplements and Medications: When to Take Them to Avoid Absorption Problems
Fiber-Medication Timing Checker
Check if your medication timing conflicts with fiber supplements. Many common medications can lose effectiveness when taken with fiber if timing isn't correct.
Key Timing Guidelines
According to medical guidelines, take fiber supplements:
- At least 1 hour before medications
- Or 2-4 hours after medications
For statins: fiber can enhance effectiveness when taken before meals
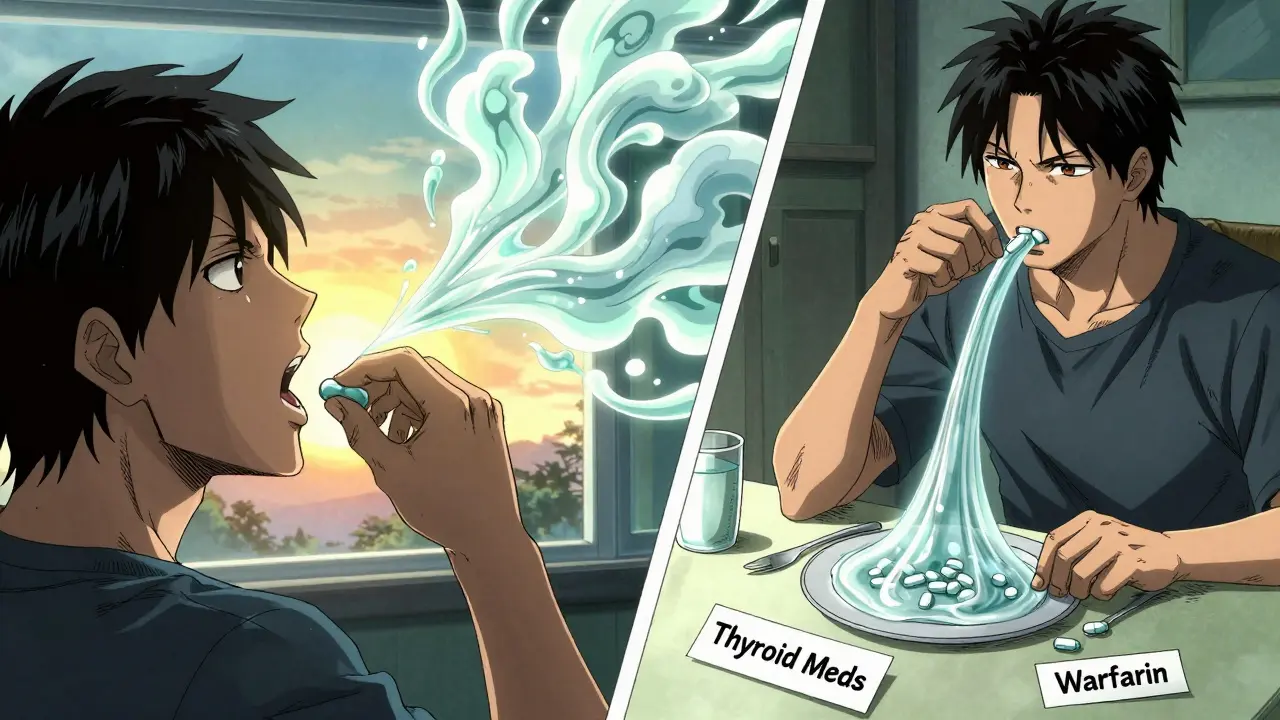
Many people take fiber supplements to feel better, manage cholesterol, or keep things moving regularly. But if you’re also on daily medications, taking fiber at the wrong time can make your pills less effective-sometimes dangerously so. It’s not just a myth. Real people have seen their thyroid levels go out of range, their blood thinners stop working, or their blood pressure spike-all because they took fiber and medicine together. The fix isn’t complicated, but it’s often overlooked.
Why Fiber Interferes with Medications
Fiber supplements like psyllium (Metamucil), methylcellulose, or inulin don’t just add bulk to your stool. When they hit your stomach and small intestine, they absorb water and turn into a thick, sticky gel. That gel doesn’t just help with digestion-it can trap medications as they try to pass through. Think of it like wrapping your pill in saran wrap before it has a chance to dissolve. The result? Less of the drug gets into your bloodstream, and your body doesn’t get the full benefit.This isn’t just theory. A 2020 study found that when people took levothyroxine (a thyroid hormone) at the same time as psyllium, their absorption dropped by nearly 29%. That’s enough to throw off thyroid control for months. Other drugs affected include warfarin (a blood thinner), metformin (for diabetes), tetracycline antibiotics, and some blood pressure medications. The American Pharmacists Association says the interaction is real, predictable, and avoidable-if you know when to separate them.
When to Take Fiber Supplements
The gold standard advice from the Mayo Clinic, Cleveland Clinic, and FDA labeling guidelines is simple: take fiber supplements at least one hour before or two to four hours after any medication. That window gives your body time to absorb the drug before the gel forms, and then lets the fiber do its job afterward.For most people, the easiest way to do this is to tie fiber to meals. If you take your medications in the morning-say, levothyroxine on an empty stomach at 7 a.m.-wait until after lunch or dinner to take your fiber. Or, if you take meds at night, take fiber in the morning. Many patients find success taking fiber right before their largest meal, because it helps with fullness and digestion. But here’s the catch: don’t take it right before bed.
Research from Hilma (2023) shows that 68% of people who took fiber within two hours of bedtime experienced bloating, gas, or stomach cramps that disrupted sleep. Metamucil, in particular, has been flagged in consumer reviews for causing nighttime discomfort. One user on Amazon wrote, “I started taking it before bed and couldn’t sleep for three nights straight.” That’s not worth the trade-off.
Medications That Definitely Don’t Mix
Not all medications are equally affected. But these ones need special attention:- Levothyroxine (for hypothyroidism): Even a small drop in absorption can mean your TSH levels climb, leading to fatigue, weight gain, or depression. One nurse on Reddit shared a case where a patient’s TSH stayed high for months-until they separated fiber and thyroid meds by four hours. Levels normalized in six weeks.
- Warfarin (blood thinner): If your INR levels start fluctuating without reason, fiber timing could be the culprit. A change in absorption can increase bleeding risk or cause clots.
- Metformin (diabetes): Fiber can slow its absorption, which might sound good for blood sugar control-but it can also lead to unpredictable spikes or lows if you’re not monitoring closely.
- Tetracycline and other antibiotics: Fiber can bind to these drugs and stop them from working, turning a short course into a prolonged infection.
- Some blood pressure meds: Beta-blockers and calcium channel blockers have shown reduced effectiveness when taken with fiber, especially psyllium.
Keep a list of your meds and check the patient information leaflet. Many now include a warning about fiber interactions. If it doesn’t say anything, ask your pharmacist. Don’t assume it’s safe.

When Fiber Actually Helps Medications
There’s one big exception: statins. Research published in PMC (2015) found that combining a low dose of simvastatin (10 mg) with 15 grams of psyllium per day-taken before meals-lowered LDL cholesterol by 63%, better than the statin alone. This isn’t a fluke. The fiber helps trap bile acids, forcing the liver to pull more cholesterol from the blood. The result? A stronger effect with less drug.This doesn’t mean you should start mixing them on your own. But if you’re on a statin and your doctor knows you’re using fiber, they might adjust your plan. Always talk to your provider before combining them. The key here is timing: taking fiber before meals, not hours apart, is what makes this synergy work.
Special Cases: Bariatric Surgery and IBS
People who’ve had weight-loss surgery face unique challenges. Their stomachs are smaller, their digestion is faster, and their nutrient absorption is already compromised. Taking fiber too soon after meds can cause blockages or malabsorption. Experts at Bodyspec recommend starting with just 1-2 grams of fiber per day and increasing slowly. Always wait at least one hour before or two hours after any medication.If you have IBS, fiber can backfire. Some types-like inulin or chicory root-trigger gas and bloating. Bon Secours reports that 42% of IBS patients had worse symptoms when taking fiber on an empty stomach. For them, taking fiber with meals, not before, often works better. Psyllium tends to be gentler than other forms, but even then, start low and go slow.
How to Make This Easy
You don’t need to memorize a chart. Just build a simple routine.- Write down all your meds and when you take them. Include vitamins, supplements, and over-the-counter drugs.
- Identify the ones with known fiber interactions. Focus on thyroid, blood thinners, antibiotics, and blood pressure meds first.
- Choose a fiber window. If you take meds in the morning, take fiber after dinner. If you take meds at night, take fiber after breakfast.
- Use phone reminders. Set two alarms: one for your meds, one for fiber. Consistency matters more than perfect timing.
- Drink water. Always take fiber with at least 8 ounces of water. And aim for 64-80 ounces total per day. Fiber without water = constipation.
Start with a low dose-1-2 grams per day-and increase by 1 gram every few days. This cuts down on gas and bloating. Most people can reach the full 5-10 gram dose in 2-4 weeks without discomfort.

What to Do If You’ve Been Taking Them Together
If you’ve been taking fiber and your meds at the same time for weeks or months, don’t panic-but don’t ignore it either.Check your last lab results. Are your thyroid levels, INR, or blood sugar suddenly off-track? Did your doctor recently increase your dose of a medication without explaining why? These could be red flags.
Start separating them now. Wait two hours after your morning meds before taking fiber. Or take fiber in the evening, four hours before your bedtime meds. Give it at least four weeks to see if things stabilize. Then ask your doctor for a follow-up test. Many patients see improvements within 6-8 weeks.
Why This Isn’t Common Knowledge
A 2022 survey by the National Community Pharmacists Association found that only 39% of patients got clear timing instructions when buying fiber supplements. Most assume it’s “just fiber” and safe with everything. Pharmacists are busy. Labels are vague. And fiber supplements aren’t drugs-so they’re not regulated the same way.That’s why you need to be your own advocate. Don’t wait for someone to tell you. Ask your pharmacist: “Which of my medications should I avoid taking with fiber?” Write it down. Stick it on your fridge. Or set a reminder on your phone.
What’s Coming Next
Researchers are working on time-release fiber formulas that form gel more slowly-so they don’t interfere with meds. These are in Phase 2 trials and could be available in the next few years. But until then, the old advice still holds: space it out.The global fiber supplement market is growing fast-projected to hit $3.7 billion by 2030. More people are using them. And more people are getting caught off guard by interactions. You don’t have to be one of them.
Can I take fiber supplements with my morning coffee?
Yes, as long as your coffee isn’t followed by medication within the next hour. Coffee doesn’t interfere with fiber. But if you take levothyroxine or other meds on an empty stomach with water, wait at least one hour after your coffee before taking fiber. Avoid taking fiber with any drink that contains calcium or iron-those can also bind to medications.
Is psyllium the only fiber that causes problems?
No, but it’s the most common culprit because it forms the thickest gel. Methylcellulose (Citrucel) and calcium polycarbophil (FiberCon) are less viscous and may cause fewer interactions, but they still can. Don’t assume a different brand is safe. Always separate all fiber supplements from medications by at least one hour before or two to four hours after.
What if I forget and take them together?
One mistake won’t ruin your treatment, but don’t make it a habit. If you accidentally take fiber and a medication together, wait at least four hours before taking your next dose of the medication. Don’t double up. Monitor for symptoms-like unusual fatigue, dizziness, or changes in bowel habits-and mention it at your next appointment. Your doctor may want to check your blood levels.
Can I take fiber with vitamins and supplements?
Many vitamins and supplements can be affected too-especially iron, calcium, zinc, and fat-soluble vitamins like A, D, E, and K. If you take a multivitamin or mineral supplement, separate it from fiber by the same timing rules: one hour before or two to four hours after. Always check the label or ask your pharmacist.
How long does it take for fiber to stop affecting my meds?
Once you separate fiber and medication, your body will start absorbing the drug normally again within a few days. But it can take 4-6 weeks for lab values to stabilize, especially for thyroid or blood thinners. Don’t rush to change your dose-wait for your doctor’s test results. Consistency over time is what matters most.






Comments
Wren Hamley
January 4, 2026 AT 15:24So fiber’s basically a drug sponge? That’s wild. I’ve been taking Metamucil with my levothyroxine for years thinking it was ‘natural’ so it couldn’t interfere. Turns out I was just slowly turning my thyroid into a slideshow. Thanks for the wake-up call. Time to reorganize my whole damn routine.
Kerry Howarth
January 5, 2026 AT 03:01Separate fiber and meds by 1 hour before or 2–4 hours after. Simple. Effective. Done.
Neela Sharma
January 5, 2026 AT 07:24Imagine your body as a busy highway and your meds are cars trying to get through-fiber is a sandstorm that blankets the road. You don’t stop the cars, you just wait for the storm to pass. Life’s like that sometimes. Patience isn’t passive. It’s medicine.
Shruti Badhwar
January 5, 2026 AT 22:08The data presented is scientifically robust and aligns with current clinical guidelines. However, the casual tone of the article may undermine its credibility among medical professionals. Precision in language is non-negotiable in pharmacological communication.
Brittany Wallace
January 6, 2026 AT 01:17Wow. I never thought about fiber like this. 😮 I’ve been taking it before bed with my vitamins and now I’m scared. Thanks for the clarity-this is the kind of info that actually saves lives. 🙏
Michael Burgess
January 7, 2026 AT 13:04Statins + fiber = power couple. Who knew? I’ve been taking psyllium before breakfast with my simvastatin and my LDL dropped like it owed someone money. My doc was shocked. Turns out, timing isn’t just about avoiding disasters-it can unlock hidden synergies. Mind blown.
Liam Tanner
January 8, 2026 AT 03:18Good breakdown. I’d add that if you’re on multiple meds, a pill organizer with labeled time slots makes this way easier. No guesswork. Just set it and forget it.
Hank Pannell
January 10, 2026 AT 02:06It’s fascinating how something so benign-fiber-is treated like harmless fluff while it’s quietly sabotaging pharmacokinetics. We’ve normalized ‘natural’ as ‘safe,’ but biology doesn’t care about marketing. The FDA regulates aspirin like a controlled substance but lets psyllium sit next to granola bars. That’s not safety-it’s regulatory arbitrage.
veronica guillen giles
January 10, 2026 AT 14:14Oh great. So now I can’t even eat my oatmeal without a PhD in pharmacology? 🙄 Next they’ll tell me coffee ruins my antidepressants. Can we just… let people live?
Ian Ring
January 11, 2026 AT 12:01Thank you for this. I’ve been struggling with erratic INR levels for months-and now I realize I’ve been taking my fiber with my warfarin. I’m changing my routine tonight. I’ve printed this out and taped it to my fridge. 🙏
Tru Vista
January 12, 2026 AT 21:01Metamucil? Nah. I just eat flaxseed. It’s ‘natural’ so it’s fine. Also, my doc never mentioned this. Probably just pushing pharma.
JUNE OHM
January 13, 2026 AT 07:46THIS IS A BIG PHARMA LIE. Fiber doesn’t interfere with meds-THEY’RE MAKING YOU DOUBT NATURAL HEALTH. They want you to keep buying expensive pills while hiding the truth. Wake up. Eat chia. Drink water. Trust your body.
Philip Leth
January 14, 2026 AT 22:08Man, I just took fiber with my blood pressure pill this morning. Guess I’m gonna be dead by Friday. 😎 Just kidding. But seriously, I’m switching to after dinner now. Thanks for the heads-up.
Angela Goree
January 15, 2026 AT 17:55Why isn’t this on the label?!?!?!?! I’ve been taking this stuff for years with my meds and now I’m terrified. Someone should sue. Someone should protest. This is negligence.
Tiffany Channell
January 17, 2026 AT 17:52People still take fiber supplements? That’s like swallowing sawdust because you don’t know how to eat broccoli. This entire article is a symptom of a broken health culture. Get real food. Stop buying powders. End of story.