Generic Drug Quality Issues: Manufacturing Plant Problems Explained

When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But behind that simple promise is a complex, global supply chain where quality can slip through the cracks. In 2018, the FDA found cancer-causing impurities in blood pressure meds made in China and India. That wasn’t an isolated case. Since then, over 3,900 drug products have been recalled due to manufacturing flaws - and most of them were generics.
What Goes Wrong in Generic Drug Factories?
Generic drugs aren’t made in labs with white coats and pipettes. They’re made in factories - often overseas - where pressure to cut costs can override safety. The core problem? Failure to follow Current Good Manufacturing Practices (cGMP). These aren’t suggestions. They’re legal requirements. When a factory skips steps - like not validating equipment, skipping stability tests, or falsifying records - the drug can become unsafe.Common issues include:
- Nitrosamine impurities: Carcinogens accidentally formed during chemical reactions. Found in valsartan, metformin, and ranitidine - leading to global recalls.
- Inconsistent dissolution: The pill doesn’t break down properly in your body. One batch might release the drug too fast; another too slow. This is especially dangerous for heart meds like nitroglycerin or immunosuppressants like tacrolimus.
- Poor packaging: Moisture or light exposure can degrade the drug before you even take it. One inspection found bottles with cracked seals and labels peeling off.
- Unreliable testing methods: Labs use faulty instruments or skip quality checks. In 2022, 18.7% of FDA warning letters cited inadequate analytical methods.
- Dirty or outdated equipment: Rust, residue, and cross-contamination from previous batches. One Indian plant was caught dumping quality control documents into acid.
These aren’t hypotheticals. They’re documented in FDA inspection reports. A 2022 inspection of an Intas Pharmaceuticals facility in Gujarat showed an employee pouring acid into a trash can full of testing records. That’s not a mistake. That’s intentional fraud.
Why Are Foreign Plants More Problematic?
Eighty percent of the active ingredients in your pills come from outside the U.S. - mostly China and India. But inspections there are not the same as in the U.S.In America, the FDA shows up unannounced. In foreign countries, they give notice - sometimes weeks in advance. That gives factories time to clean up, hide problems, or even fabricate records. A 2023 Ohio State study found that generic drugs made in India were linked to 23.7% more severe side effects than those made in the U.S.
The numbers back it up:
- Chinese facilities get 28.6% more FDA inspection violations than U.S. ones.
- Indian facilities get 19.3% more.
- Only 13% of foreign drug plants are inspected each year - despite making 73% of finished drugs sold in the U.S.
And here’s the kicker: the FDA tests just 0.02% of imported drug shipments in the lab. That means 99.98% of pills enter the country without being checked for purity, potency, or contamination.

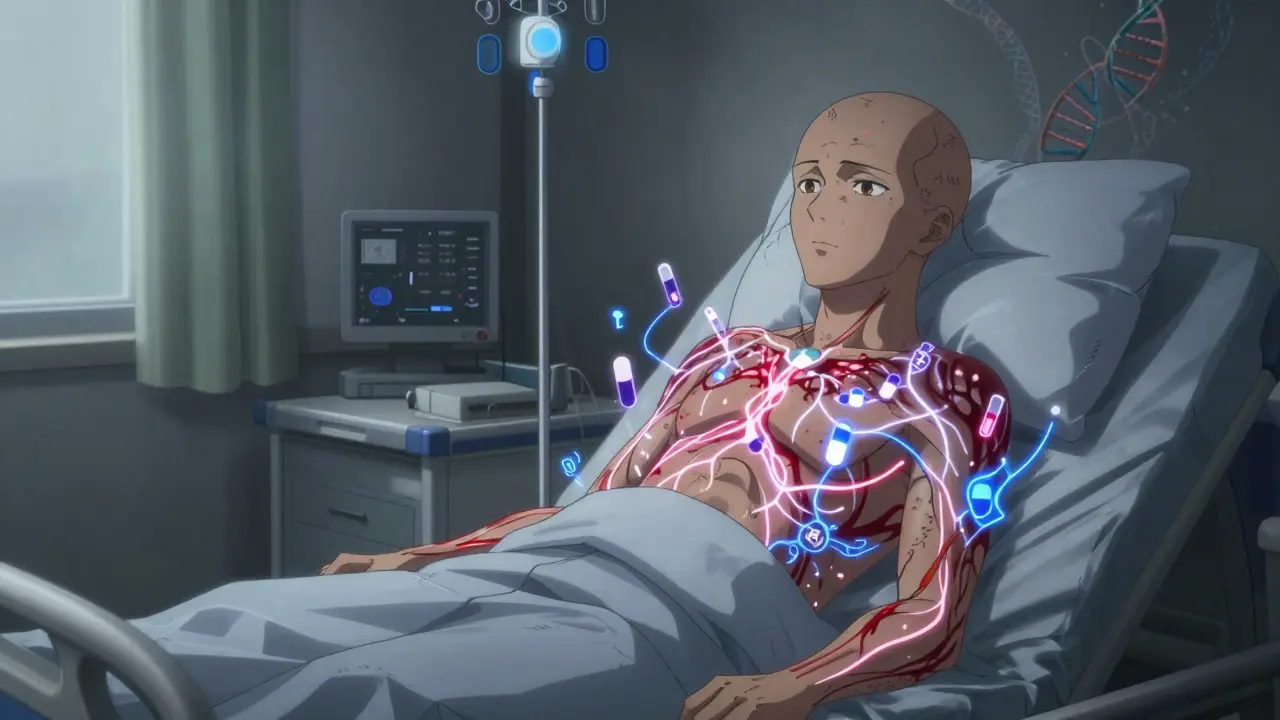
Who’s Affected - And How?
It’s not just about recalls. It’s about what happens when a drug doesn’t work - or makes you sick.Therapeutic failure is real. A 2022 survey of hospital pharmacists found that 67.3% had seen at least one patient’s condition worsen after switching to a generic. Over 40% blamed products from India. Patients reported generic valsartan as “ineffective” - 3.2 stars on Drugs.com compared to 4.1 for the U.S.-made version.
Narrow Therapeutic Index (NTI) drugs are the most dangerous. These are meds where a tiny difference in dose can cause serious harm - like warfarin, levothyroxine, or cyclosporine. In 2022, 37% of FDA rejection letters for generic approvals were for NTI drugs. Why? Because proving they’re equivalent to the brand name is harder - and many factories aren’t equipped to do it right.
FAERS, the FDA’s adverse event database, logged 1,842 reports tied to generic drug quality between 2019 and 2022. One company, Impax Laboratories, accounted for 14.3% of those reports - all because their nitroglycerin tablets didn’t dissolve properly. Patients had heart attacks because the drug didn’t reach their bloodstream.
Why Is This Still Happening?
It’s not just about bad actors. It’s about broken economics.Generic drug prices have dropped 18.3% every year since 2018. To stay profitable, manufacturers cut corners. Quality control budgets fell by 22.7% in that same period. Training? Reduced. Equipment upgrades? Delayed. Staffing? Underpaid. Data integrity? Ignored.
Only 23.8% of generic makers use Quality by Design (QbD) - a system that builds safety into the product from day one. It’s expensive. It takes 18-24 months to implement. And it costs an average of $2.7 million per plant. Most companies won’t spend it.
Even the FDA is stretched thin. Its budget for foreign inspections increased by $56.7 million in 2022 - but that still only gets them to 1,800 inspections a year by 2027. There are nearly 3,000 foreign drug plants. That’s one inspection every 1.7 years per facility. On average.

What’s Being Done - And Is It Enough?
There are signs of change. The European Medicines Agency now does unannounced inspections at all foreign facilities. Since January 2023, critical findings jumped 41.2%. The FDA is moving toward risk-based inspections - targeting high-risk drugs and high-risk plants first.The 2023 Drug Competition Action Plan demands more testing for complex generics - 75% more bioequivalence studies, 100% more stability data. That’s good. But it’s reactive. It doesn’t stop bad drugs from reaching patients. It just makes them harder to approve after the damage is done.
Meanwhile, the top 10 generic manufacturers now control 58.4% of the U.S. market. That’s consolidation - and with consolidation comes power. But also risk. If one big player cuts corners, millions of prescriptions are affected.
And the White House now calls pharmaceutical supply chains a national security issue. Over 72% of essential medicine ingredients come from China and India. What happens if those countries restrict exports? Or if a factory shuts down because of a quality scandal?
What You Can Do
You can’t inspect a factory. But you can be informed.- Check recalls: Visit fda.gov/drugs/drug-safety-and-availability and search your medication.
- Ask your pharmacist: If your generic switched brands unexpectedly, ask why. Was it a recall? A shortage? A quality issue?
- Report side effects: Use the FDA’s MedWatch program. One report might be ignored. Ten thousand? That’s a pattern.
- Don’t assume all generics are equal: Some brands are made by reputable manufacturers. Others aren’t. Your pharmacist can tell you which ones have better track records.
Generic drugs saved the U.S. healthcare system hundreds of billions. But safety can’t be sacrificed for savings. If a pill doesn’t work - or makes you worse - it’s not a generic. It’s a risk.
Are generic drugs less effective than brand-name drugs?
Most generics work just as well as brand-name drugs. But not all. When manufacturers cut corners on quality control, testing, or packaging, the drug may not dissolve properly or may contain harmful impurities. Studies show that 15.2% of generics on the FDA Watch List have measurable differences in how they perform in the body - especially for narrow therapeutic index drugs like warfarin or thyroid medication.
Why are so many drug quality issues linked to India and China?
India and China produce 80% of the world’s active pharmaceutical ingredients and 40% of finished drugs. But FDA inspections there are scheduled in advance, giving factories time to hide problems. U.S. facilities are inspected unannounced. Foreign plants also face lower labor costs, which can lead to undertrained staff and poor data practices. In 2022, Chinese facilities had 28.6% more FDA violations than U.S. ones, and Indian facilities had 19.3% more.
How does the FDA catch bad generic drugs?
The FDA inspects manufacturing plants, reviews data submissions, and monitors adverse event reports. But they test only 0.02% of imported drug shipments in the lab. Most detection happens after patients report side effects or hospitals notice inconsistent results. The FDA also issues warning letters after inspections - but by then, millions of doses may already be in circulation.
Can I tell if my generic drug is from a bad manufacturer?
You can’t tell by the label alone. But you can ask your pharmacist. Some manufacturers have better reputations. If your drug suddenly stops working or causes new side effects after a refill, it could be a different maker. Check the FDA’s recall list or use Drugs.com to compare patient reviews of different generic brands.
What’s being done to fix this problem?
The FDA is increasing foreign inspections and prioritizing high-risk facilities. The European Medicines Agency now conducts unannounced inspections - and has seen a 41.2% spike in critical findings. New rules require more testing for complex generics. But progress is slow. Without mandatory lab testing of imports and real-time data sharing from manufacturers, the system remains vulnerable.



Comments
Diane Tomaszewski
November 16, 2025 AT 00:00It’s scary how much we just trust pills without knowing where they come from. I never thought about how packaging or moisture could ruin a drug before reading this. My grandma’s blood pressure med stopped working last year-she never said why. Now I wonder.
Latrisha M.
November 17, 2025 AT 03:12Check your pharmacy’s generic brand. Some are made by the same companies as brand-name drugs-just under a different label. Ask for the manufacturer code on the bottle. It’s not hard, and it could save your life.
Jamie Watts
November 18, 2025 AT 19:21People act like generics are all the same but no they’re not. I’ve had three different versions of metformin and two of them made me feel like I was drowning in my own sweat. One worked fine. The others? Total garbage. You can’t tell from the label. That’s the point.
John Mwalwala
November 19, 2025 AT 13:59Look at the FDA’s warning letters. They’re public. You can see exactly which plants got nailed for falsifying data. I’ve got a spreadsheet. If you’re on a narrow therapeutic index drug like warfarin or levothyroxine, cross-reference your batch with the inspection reports. It’s not paranoia-it’s survival.
Rachel Wusowicz
November 19, 2025 AT 23:29They’re not just cutting corners-they’re burying evidence. Acid in the trash can? That’s not a mistake. That’s a war crime. And the FDA? They’re playing whack-a-mole with a toothpick. They inspect 13% of foreign plants? That’s not oversight-that’s a joke. I bet the people who run these plants laugh at the idea of an unannounced inspection. They’ve got months to scrub everything clean. Meanwhile, your kid’s asthma inhaler? Could be full of asbestos dust and no one will ever know until it’s too late. I’m not saying the world’s ending. I’m saying it’s already been poisoned-and we’re the ones swallowing it.
Daniel Stewart
November 21, 2025 AT 16:31It’s fascinating how we outsource our health to nations with different cultural attitudes toward regulation. In the West, we expect perfection. In parts of Asia, efficiency trumps precision. The result? A system where profit is the only metric that matters. And we’re the ones paying the price-in blood, in hospital bills, in grief.
Oyejobi Olufemi
November 22, 2025 AT 09:29Let me tell you something. This isn’t about drugs. This is about power. Who controls your medicine? Who controls your life? China and India don’t care if you die-they care about their GDP. The FDA is a puppet. The White House is asleep. And you? You’re still buying the cheapest pill because you can’t afford the brand. Wake up. This is colonialism with a pharmacy sticker.
Ankit Right-hand for this but 2 qty HK 21
November 23, 2025 AT 03:31India makes 40% of the world’s generics. You think we don’t know how to make medicine? We’ve been making it since Ayurveda. The FDA is jealous. They can’t compete with our cost. So they cry foul. But their own plants? They’ve got more violations than we do. Stop blaming us. Fix your own broken system.
Danish dan iwan Adventure
November 23, 2025 AT 19:58Manufacturing deviations > 5% Cpk for dissolution profile = non-compliance. cGMP non-conformance in 78% of Indian facilities cited in 2023 FDA reports. Nitrosamine formation kinetics uncontrolled in 62% of ARB batches. QbD adoption <25%. End of story.
ZAK SCHADER
November 25, 2025 AT 04:21Why do we even let foreign countries make our pills? We got the best scientists, the best labs, the best tech. We outsource our meds like we outsource our customer service. Idiots. If this was cars or planes, we’d shut it down. But pills? Nah. Let the Chinese and Indians do it. Then cry when grandma dies. Typical.
Melanie Taylor
November 26, 2025 AT 10:21OMG this is so real 😭 I just found out my generic levothyroxine is from a plant that got a warning letter last year. I switched back to brand name and my energy came back in 3 days. I’m not paying $50 a month for a pill that makes me feel like a zombie. I’m done. 💔
Deepak Mishra
November 28, 2025 AT 04:02Brooooooo I had a heart attack last year because my nitroglycerin didn’t dissolve! I went to the ER and the pharmacist said ‘oh that’s the new batch from Intax’-I was like WHAT?!?!?!! I’m crying right now. My mom’s on warfarin and I won’t let her take anything but the brand name anymore. Please someone help us. 😭💊
Dan Angles
November 28, 2025 AT 19:21The systemic failure here is not merely regulatory-it is epistemological. We have outsourced not just production, but the very epistemic authority over therapeutic equivalence. The patient becomes the final, untrained sensor in a broken feedback loop. Without mandatory batch-level bioequivalence testing and real-time adverse event correlation, we are not practicing medicine-we are conducting a mass, uncontrolled experiment.
David Rooksby
November 28, 2025 AT 20:39Okay so here’s the thing nobody’s saying-this isn’t just about India or China. It’s about the fact that we turned pharmaceuticals into a commodity. Like toilet paper. You want cheap? You get cheap. And cheap means corners cut, records forged, labs skipped, and patients used as test subjects. The FDA doesn’t have the money. The companies don’t have the incentive. And the public? We’re too busy scrolling TikTok to care until someone we love gets sick. Then we blame the manufacturer. But the real villain? Us. We demanded cheap. We got it. And now we’re surprised when the medicine doesn’t work? Wake up. This was predictable. This was inevitable. And it’s not going to stop until we stop pretending we can outsource safety.
Teresa Smith
November 29, 2025 AT 03:08While the systemic risks outlined here are deeply concerning, the solution lies not in nationalism or fear, but in transparency and accountability. The FDA must mandate public, real-time access to inspection reports, batch-level testing data, and manufacturer compliance histories. Patients deserve to know not just what they’re taking, but who made it, where, and under what conditions. Without this, we are not consumers-we are subjects in a broken system. Policy change is possible, but only if we demand it-not with outrage, but with organized, informed pressure.