Why Generic Drug Prices Vary So Much Between U.S. States

Have you ever filled a prescription for a generic drug and been shocked by the price-only to find out your friend in another state paid a third of what you did? It’s not a mistake. It’s not a glitch. It’s the reality of how generic drug pricing works in the U.S. The same pill, made by the same factory, sold in the same dose, can cost three times more in one state than another. And the reasons? They’re not about quality, supply, or demand. They’re about hidden systems, legal loopholes, and who’s pulling the strings behind the scenes.
Why the Same Drug Costs More in Some States
Generic drugs are supposed to be cheap. After all, they’re copies of brand-name drugs that have lost patent protection. The whole point is to slash prices. But here’s the catch: the price you pay at the pharmacy isn’t the price the pharmacy pays. It’s not even the price the manufacturer charges. It’s a tangled web of middlemen, contracts, and state-level rules that nobody talks about.
In California, a 90-day supply of generic atorvastatin (the cholesterol drug) might cost $45 with insurance. In Texas, the same prescription could cost $120. Why? Because each state has different rules for how Medicaid and private insurers reimburse pharmacies. Some states use the National Average Drug Acquisition Cost (NADAC), which updates monthly and reflects what pharmacies actually pay. Others use outdated benchmarks that don’t match reality. That gap? That’s where prices balloon.
The Hidden Players: PBMs and Their Game
Behind almost every price difference is a Pharmacy Benefit Manager-or PBM. These companies act as middlemen between drug manufacturers, insurers, and pharmacies. They negotiate prices, set formularies, and collect rebates. But here’s the problem: their business model isn’t built on lowering costs. It’s built on obscuring them.
PBMs often get paid through spread pricing. That means they tell your insurer the drug costs $100. They tell the pharmacy they’ll pay $60. They pocket the $40 difference. And because most states don’t require transparency about these spreads, you never see it. A 2022 study from the USC Schaeffer Center found that U.S. consumers overpay for generics by 13% to 20% because of these hidden markups. And it’s worse in states with weak oversight.
States like Vermont and California passed laws requiring PBMs to disclose their pricing practices. In those states, patients pay 8-12% less on average. But in states with no such laws, PBMs operate in the dark. And they profit from that darkness.
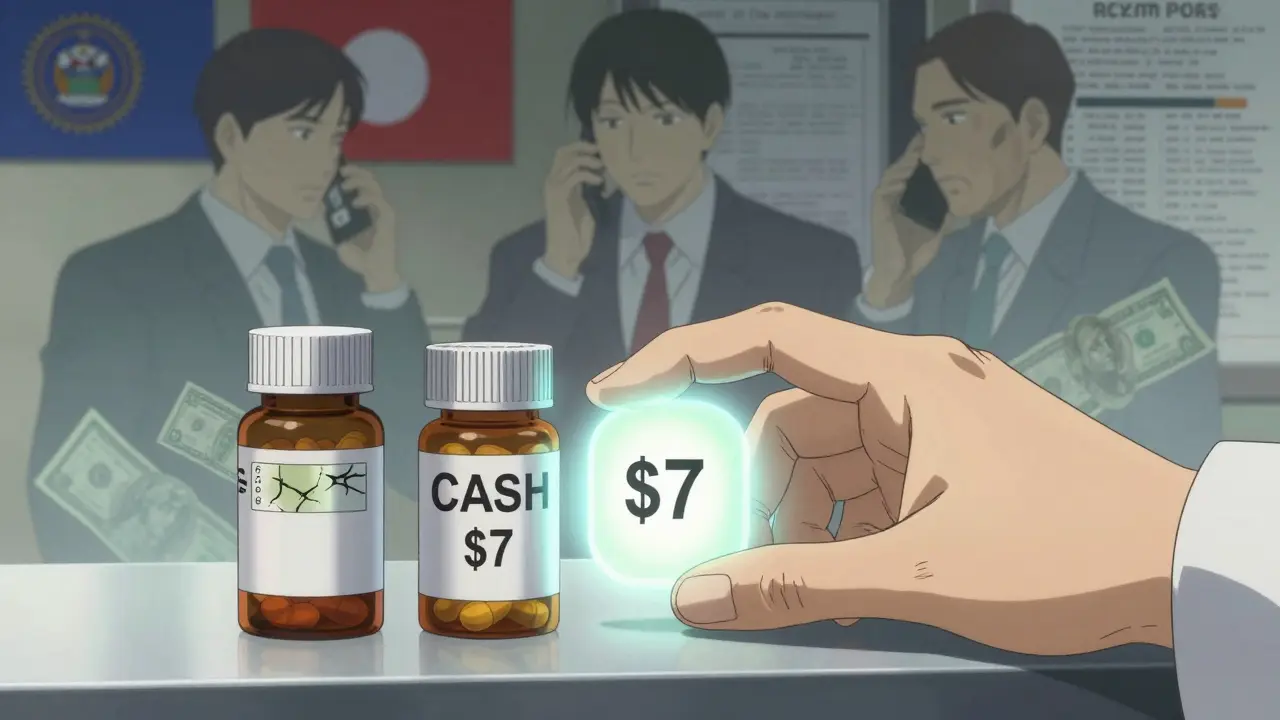
Cash vs Insurance: The Real Savings Secret
Here’s one of the biggest surprises: if you’re paying for a generic drug with insurance, you’re often paying more than if you paid cash.
Why? Because your insurance plan has a contract with a PBM that sets your copay. But that copay isn’t based on the actual cost of the drug-it’s based on the PBM’s negotiated rate, which may be inflated. Meanwhile, pharmacies that accept cash payments-like Mark Cuban’s Cost Plus Drug Company or Blueberry Pharmacy-buy drugs directly from manufacturers and charge a flat markup. No middlemen. No spreads. No hidden fees.
GoodRx data from 2022 showed that for the same generic drug, cash prices were 30% to 70% lower than insurance copays. And in states with fewer pharmacies, like rural areas of Nebraska or West Virginia, the cash savings can be even bigger. That’s why 4% of all generic prescriptions in 2020 were paid in cash-97% of those were for generics. People figured it out. They just needed a way to find the price.
State Laws: Some Help, Some Backfire
States have tried to fix this. Maryland passed a law in 2017 that capped generic drug prices to prevent “price gouging.” It worked-for a while. Then a federal court struck it down, saying states can’t regulate prices that cross state lines. Nevada tried targeting diabetes drug prices. The lawsuit was dropped. Why? Because manufacturers and PBMs threatened to sue under the Defend Trade Secrets Act, claiming the state was stealing their pricing data.
So now, states are shifting tactics. Instead of setting price caps, they’re pushing for transparency. California requires PBMs to report their spreads. New York mandates that pharmacies tell you the cash price before you pay. These aren’t perfect fixes, but they give consumers tools to fight back.
Meanwhile, 18 states have created drug affordability boards as of 2023. These panels review drug prices and recommend action. But they can’t force anyone to lower prices. They’re advisory. And they’re slow. So while they look good on paper, they don’t stop your prescription from costing $150 this month.
Medicare’s Cap Doesn’t Fix Everything
The Inflation Reduction Act of 2022 capped insulin at $35 a month and will cap total out-of-pocket drug spending at $2,000 a year starting in 2025. Sounds great, right? But here’s the catch: it only applies to Medicare Part D beneficiaries. That’s about 32% of U.S. drug spending.
If you’re under 65 and get insurance through your job, you’re not covered. If you’re on Medicaid, your state’s rules still apply. If you’re uninsured, you’re on your own. And even for Medicare patients, the cap doesn’t touch the underlying price differences between states. You might pay $35 for insulin, but if your blood pressure pill costs $80 in Florida and $25 in Minnesota, you’re still stuck with the gap.
What You Can Do Right Now
Don’t wait for your state to fix this. You can take control today.
- Always ask for the cash price before using insurance.
- Use GoodRx, SingleCare, or RxSaver to compare prices at nearby pharmacies.
- If your pharmacy doesn’t list cash prices, call other pharmacies in your area. Prices can vary by 50% within the same city.
- Switch to a cash pharmacy if your state has one. These pharmacies often charge 70% less than insurance copays.
- Check if your state has a drug affordability board or transparency law. If so, use their price lookup tools.
For example, in Ohio, a 30-day supply of metformin might cost $18 with insurance. But the cash price at a local pharmacy is $7. That’s not a typo. That’s the system working as designed-for someone else’s profit.
The Bigger Picture: Why This Keeps Happening
Generic drugs make up 90% of prescriptions in the U.S. But they account for only 18% of total drug spending. That means the system isn’t broken because generics are expensive. It’s broken because the middlemen are making money off how they’re priced.
The U.S. spends 2.78 times more on prescription drugs than other wealthy countries. And state-by-state variation is part of why. While Canada or Germany have national pricing systems, the U.S. lets each state-and each PBM-set its own rules. The result? A patchwork of unfairness.
And here’s the worst part: the companies making billions from this system aren’t drugmakers. They’re the PBMs, the insurers, and the pharmacy chains that benefit from opacity. The manufacturers? They’re often selling generics for pennies. The real gouging happens downstream.
Until states enforce real transparency-or Congress steps in with federal price standards-this won’t change. But until then, you have more power than you think. Know your options. Shop around. Pay cash when it makes sense. And don’t assume your insurance is helping you. Sometimes, it’s the reason you’re paying so much.




