Hyponatremia from SSRIs: How Low Sodium and Confusion Risk Affect Antidepressant Use
SSRI Hyponatremia Risk Calculator
Risk Assessment Form
Risk Assessment Results
When you start an SSRI for depression, you expect to feel better - not confused, dizzy, or suddenly unable to think clearly. But for some people, especially older adults, the very medication meant to lift their mood can trigger a dangerous drop in sodium levels. This isn’t rare. It’s not a myth. It’s a well-documented, preventable risk tied directly to how SSRIs interact with your body’s water balance.
What Exactly Is Hyponatremia?
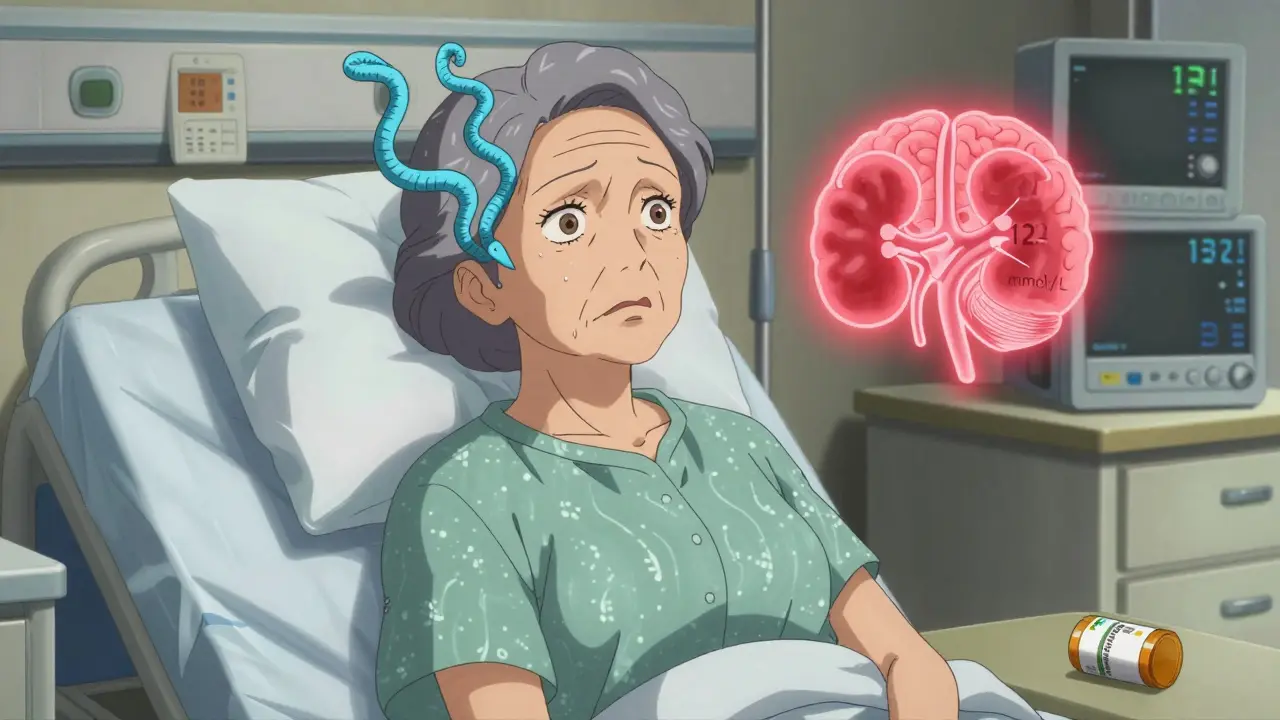
Hyponatremia means your blood sodium is too low - below 135 mmol/L. Sodium isn’t just table salt. It’s a key electrolyte that helps your nerves, muscles, and brain work right. When sodium drops too far, water floods into your cells, including brain cells. That’s when things get serious: confusion, headaches, nausea, seizures, and in extreme cases, coma or death.Studies show that SSRIs - drugs like citalopram, sertraline, fluoxetine, and paroxetine - are among the most common causes of drug-induced hyponatremia. In people over 65, the risk jumps to nearly 1 in 6. That’s not a small number. It’s a major safety issue.
Why Do SSRIs Lower Sodium?
It comes down to serotonin. SSRIs boost serotonin in your brain to improve mood. But serotonin also acts on your hypothalamus - the part of your brain that controls antidiuretic hormone (ADH). Too much serotonin = too much ADH. That tells your kidneys to hold onto water instead of flushing it out.Result? Your body keeps water, but sodium stays the same. So your blood gets diluted. Sodium levels sink. This is called SIADH - syndrome of inappropriate antidiuretic hormone secretion. It’s not a side effect you can just ‘tough out.’ It’s a physiological chain reaction that starts within days of starting or increasing an SSRI dose.
Who’s at Highest Risk?
Not everyone on SSRIs gets hyponatremia. But certain people are far more vulnerable:- Age 65+: Risk triples. The older you are, the less your kidneys can adjust to fluid shifts.
- Women: Over 65% of reported cases are in women, likely due to lower body weight and hormonal differences.
- Low body weight (under 60 kg): Less total body water means even small fluid changes have bigger effects.
- Renal impairment: If your eGFR is below 60, your kidneys can’t clear excess water efficiently.
- On diuretics: Especially thiazides. Taking a water pill with an SSRI increases hyponatremia risk by over four times.
- Starting or increasing dose: The biggest spike in risk happens in the first two to four weeks.
One case from a Reddit caregiver in March 2024 described her 82-year-old mother becoming severely confused two weeks after starting citalopram. Sodium dropped to 122 mmol/L. She was hospitalized. The medication was stopped. It took days to recover. This isn’t unusual.
Which SSRIs Are Most Dangerous?
Not all SSRIs carry the same risk. Data from the 2024 European Psychiatry meta-analysis shows clear differences:| Medication | Risk vs. Non-SSRI | Notes |
|---|---|---|
| Citalopram | 2.37x higher | Highest risk among SSRIs |
| Sertraline | 2.15x higher | Commonly prescribed, high incidence |
| Fluoxetine | 1.98x higher | Long half-life - risk persists |
| Paroxetine | 1.82x higher | Strong anticholinergic effects add complexity |
| Mirtazapine | 0.47x (lower) | Safest alternative for elderly |
| Bupropion | 0.85x (lower) | Non-serotonergic - minimal hyponatremia risk |
| Venlafaxine (SNRI) | 1.72x higher | Still higher than mirtazapine |
For every 1,000 people treated with SSRIs, about 19 develop hyponatremia. With mirtazapine? Only 7. That’s a number needed to harm (NNH) of 82 - meaning you’d have to treat 82 people with an SSRI instead of mirtazapine to cause one extra case of low sodium.
What Do Symptoms Look Like?
Early signs are often mistaken for aging, dementia, or just ‘getting older.’ That’s the problem.- Mild: Headache, nausea, fatigue, loss of appetite
- Moderate: Confusion, trouble concentrating, dizziness, muscle weakness
- Severe: Seizures, slurred speech, loss of coordination, coma
One study found patients waited an average of 7.2 days before their hyponatremia was correctly diagnosed. In elderly patients, doctors often assume confusion is Alzheimer’s or just depression worsening - not a drug reaction. That delay can be deadly.
What Should Doctors Do?
The American Psychiatric Association and the American Geriatrics Society now say: test sodium before starting SSRIs.- Baseline test: Do a blood test for sodium within 7 days before starting an SSRI.
- Repeat at 2 weeks: That’s when levels usually drop.
- High-risk patients: Check monthly for the first 3 months.
And here’s the kicker: 63% of primary care doctors didn’t even know the typical onset window is 2-4 weeks. If your doctor didn’t mention testing, ask. It’s simple. It’s cheap. It’s life-saving.
What If Sodium Is Already Low?
If sodium is between 125-134 mmol/L:- Stop the SSRI immediately
- Restrict fluids to 800-1000 mL per day
- Recheck sodium every 12-24 hours
- Most cases improve within 72 hours
If sodium is below 125 mmol/L - it’s an emergency. Hospitalization is required. Treatment involves slow IV infusion of 3% hypertonic saline. But here’s the catch: correcting sodium too fast can cause osmotic demyelination syndrome - a devastating brain injury. Doctors must move slowly: no more than 6-8 mmol/L increase in the first 24 hours.

What Are the Safer Alternatives?
If you’re over 65, or have kidney issues, or take diuretics - consider switching away from SSRIs.- Mirtazapine: Lowest risk. Doesn’t affect serotonin in the same way. Often used for sleep and appetite too.
- Bupropion: Works on dopamine and norepinephrine, not serotonin. Minimal hyponatremia risk.
- Nortriptyline (a TCA): Lower risk than amitriptyline. Still needs monitoring, but better than SSRIs in high-risk groups.
Between 2018 and 2023, SSRI use in people over 65 dropped 22%. Mirtazapine prescriptions for that group rose 35%. That’s not a coincidence. Doctors are learning.
Why Isn’t This Common Knowledge?
Only 28.7% of patients surveyed in 2023 said they were warned about hyponatremia before starting an SSRI. That’s unacceptable. The FDA updated SSRI labels in 2022 to include this risk. But warnings on a pill bottle don’t reach most patients. It falls to the prescriber.And here’s the reality: SSRIs are still the most prescribed antidepressants in the U.S. - over 214 million prescriptions in 2023. That means millions are still being started without sodium checks. The annual cost of hospitalizations for this preventable issue? Over $890 million in the U.S. alone.
What Should You Do?
If you or a loved one is on an SSRI:- Ask your doctor: “Have my sodium levels been checked?”
- Watch for new confusion, nausea, or headaches - especially in the first month.
- If symptoms appear, don’t wait. Get a blood test. Sodium levels can drop fast.
- If you’re over 65 and starting antidepressants, ask if mirtazapine or bupropion are options.
Depression is serious. But so is hyponatremia. You don’t have to choose between them. With the right screening and smarter choices, you can treat depression safely - without risking brain damage from low sodium.
Can SSRIs cause confusion in elderly patients?
Yes. SSRIs can cause confusion in elderly patients due to hyponatremia - low sodium levels triggered by excessive water retention. This often mimics dementia or depression worsening. Symptoms like disorientation, memory lapses, or difficulty speaking can appear within two to four weeks of starting or increasing the dose. A simple blood test can confirm low sodium, and stopping the SSRI usually reverses the confusion.
How long does it take for hyponatremia to develop after starting an SSRI?
Hyponatremia typically develops between two and four weeks after starting an SSRI or increasing the dose. The peak risk window is days 10-21. That’s why guidelines now recommend checking sodium levels at the two-week mark. Waiting longer can delay diagnosis and increase danger.
Is mirtazapine safer than SSRIs for older adults?
Yes. Mirtazapine has a significantly lower risk of hyponatremia - about half the risk of SSRIs. It doesn’t strongly stimulate serotonin receptors in the hypothalamus, so it doesn’t trigger excessive ADH release. For patients over 65, those with kidney problems, or those on diuretics, mirtazapine is often the preferred first-line antidepressant. It also helps with sleep and appetite, which are common issues in older adults.
Should I get a blood test before starting an SSRI?
If you’re over 65, have kidney disease, take diuretics, or have a low body weight - yes. The American Psychiatric Association recommends baseline sodium testing before starting any SSRI in high-risk patients. Even if you’re younger, asking for a test is reasonable. It takes five minutes and can prevent hospitalization.
Can hyponatremia from SSRIs be reversed?
Yes, if caught early. Stopping the SSRI and restricting fluids usually brings sodium levels back to normal within 72-96 hours. In severe cases (below 125 mmol/L), hospital treatment with slow IV saline is needed. Recovery is common, but if sodium is corrected too quickly, it can cause permanent brain damage. That’s why medical supervision is critical.
Hyponatremia from SSRIs isn’t a glitch. It’s a predictable, preventable outcome. The science is clear. The tools exist. What’s missing is routine action. If you’re prescribing, testing, or taking these drugs - don’t wait for confusion to become a crisis. Ask the question. Get the test. Choose the safer option. Your brain will thank you.






Comments
Marian Gilan
January 27, 2026 AT 09:29so u know what's REALLY happening? SSRIs are just a gateway drug for Big Pharma to get you hooked on hospital visits. they don't care if you get confused or die - they just want your insurance to pay for the IV bags. i saw a guy on youtube say the FDA knew about this since 1998 and buried it. now they're selling mirtazapine like it's magic. same company. same playbook. 🤡
Conor Murphy
January 27, 2026 AT 14:12this is so important 😔 my grandpa started sertraline and went from sharp as a tack to forgetting his own name in 3 weeks. the doctor just said 'oh he's getting old' - no blood test, no nothing. thank you for putting this out there. please share this with every elder you know. 💙
Conor Flannelly
January 27, 2026 AT 20:26the real tragedy isn't just the hyponatremia - it's how we've normalized medical neglect in geriatric care. we diagnose dementia before we check electrolytes. we assume confusion is 'just aging' before we ask if they're on SSRIs. this isn't a pharmacology issue - it's a cultural one. we've trained doctors to treat symptoms, not systems. and patients? we tell them to 'be patient' while their brain slowly swells. it's not malice - it's inertia. and inertia kills. 🤔
Patrick Merrell
January 29, 2026 AT 07:15if you're over 65 and on an SSRI and you haven't had your sodium checked, you're basically playing russian roulette with your brain. stop being lazy. get tested. or don't. but don't act surprised when you start talking to your cat like it's your therapist. 🤬
Napoleon Huere
January 29, 2026 AT 10:41this is the kind of post that makes me believe in the possibility of rational healthcare. people think depression is just 'chemical imbalance' - but this shows it's a whole-body system failure. SSRIs aren't magic pills - they're biochemical levers. and like any lever, if you pull too hard in the wrong place, the whole machine breaks. we need more posts like this. not less.
Shweta Deshpande
January 30, 2026 AT 07:07hi! i just wanted to say how much i appreciate this post 💖 i'm a nurse in Mumbai and we see this all the time - elderly patients brought in confused, family blames dementia, turns out it's citalopram from the local pharmacy. no lab, no follow-up, just a script. i always ask: 'did you get a blood test?' and 9/10 times they say 'no'. i wish i could hand out flyers at every pharmacy. maybe i'll start. also, mirtazapine is a godsend for sleep and appetite - and yes, it doesn't wreck sodium. if you're scared of side effects, try it. you won't regret it. 🌸
Neil Thorogood
January 30, 2026 AT 21:32so let me get this straight… we’ve got millions of elderly people on SSRIs, zero mandatory sodium tests, and doctors who think ‘confusion’ means ‘old age’? 🤦♂️ and you’re telling me the solution is… asking nicely? nope. we need a law. mandatory baseline labs before any SSRI. like seatbelts. like helmets. if your doctor says no, find a new one. your brain isn’t optional.
Jessica Knuteson
January 31, 2026 AT 15:18the data is solid but the framing is performative. everyone knows SSRIs have risks. the real issue is that depression is treated like a virus to be eradicated, not a human condition to be held. you don't fix confusion by testing sodium. you fix it by listening. but that's harder than writing a script.