Glomerulonephritis: How Your Immune System Attacks Kidney Filters
Imagine your kidneys are like tiny coffee filters, cleaning your blood 24/7. Now imagine your immune system, the body’s defense team, suddenly turns on those filters and starts attacking them. That’s glomerulonephritis - a condition where your own immune system damages the microscopic filtering units in your kidneys, called glomeruli. It’s not just a rare disease. It affects about 12.5 out of every 100,000 people in the U.S. every year, and it’s one of the top causes of kidney failure in younger adults.
What Happens Inside Your Kidneys When GN Strikes
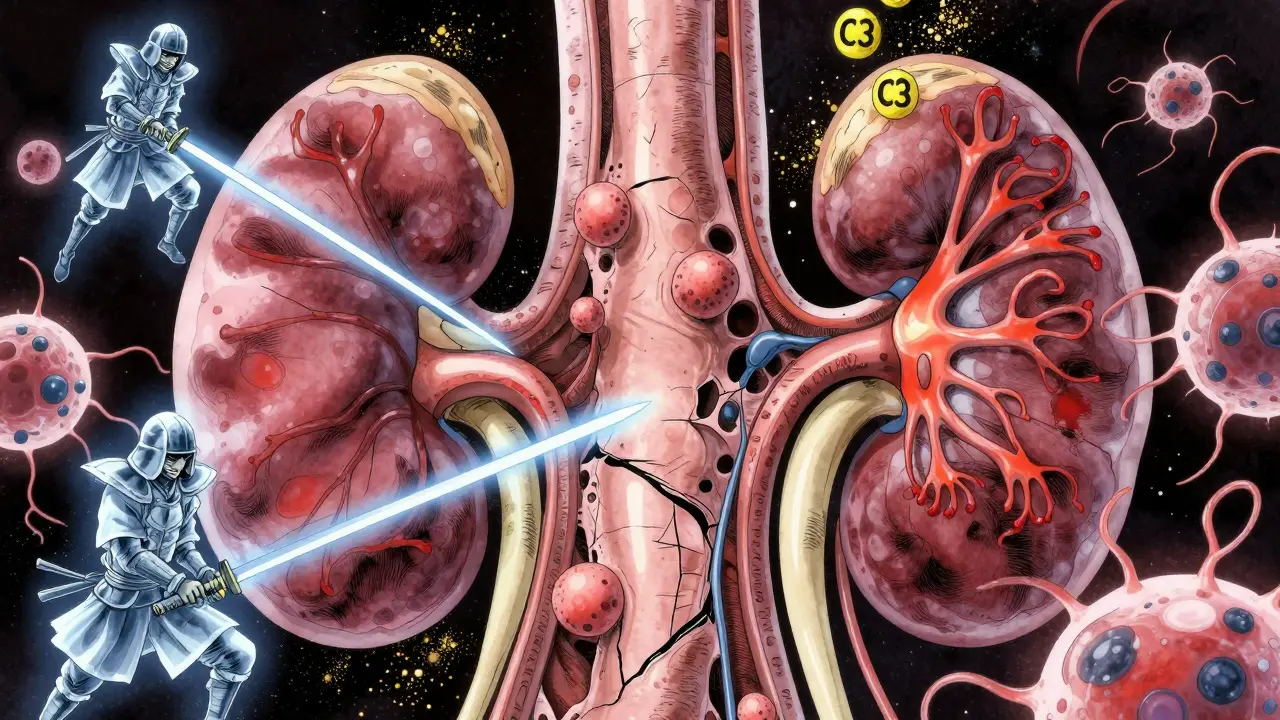
Your kidneys don’t just remove waste. They also balance fluids, control blood pressure, and keep essential proteins in your blood. Each kidney has about a million glomeruli - tiny clusters of capillaries wrapped in a protective mesh of cells. These are the filters. They’re made of three layers: the endothelial cells lining the blood vessels, the basement membrane (a structural scaffold), and the podocytes - specialized cells that act like tiny feet gripping the filter. In glomerulonephritis, the immune system sends antibodies or immune complexes to attack one or more of these layers. Sometimes it’s the basement membrane. Other times, it’s the podocytes. When podocytes get damaged, they can’t hold onto proteins anymore. That’s why you start losing large amounts of protein in your urine - a sign of nephrotic syndrome. Other times, red blood cells leak through the damaged filter, causing blood in the urine - a hallmark of nephritic syndrome. The damage isn’t always obvious at first. Many people don’t feel sick until their kidneys are already struggling. Fatigue is the most common complaint, reported by 65% of patients. Swelling in the legs, ankles, or face from fluid retention is another early warning sign. High blood pressure often follows as the kidneys lose their ability to regulate fluid and salt.The Two Main Types: C3 Glomerulonephritis and Immune Complex-Mediated MPGN
Not all glomerulonephritis is the same. Two major types dominate the clinical picture: C3 glomerulonephritis (C3G) and immune complex-mediated membranoproliferative GN (IC-MPGN). C3G is driven by a broken complement system - a part of the immune system that normally helps clear infections. In C3G, the complement system goes haywire. It starts activating nonstop, flooding the glomeruli with C3 protein. Biopsies show C3 deposits 3 to 5 times higher than normal. About 60-70% of C3G cases involve autoantibodies called C3 nephritic factor, which tricks the immune system into thinking it’s under attack. IC-MPGN, on the other hand, is caused by immune complexes - clumps of antibodies and antigens - getting stuck in the glomeruli. These are often leftovers from past infections like hepatitis or malaria, or they can form in autoimmune diseases like lupus. In 95% of IC-MPGN cases, electron microscopy reveals dense deposits in the filter walls. The difference matters because treatment isn’t one-size-fits-all. C3G responds poorly to standard steroids. IC-MPGN might improve with immunosuppressants - but only if caught early.Common Forms of GN You Should Know
IgA nephropathy is the most common form of primary glomerulonephritis worldwide. It happens when IgA antibodies - normally used to fight gut infections - build up in the kidneys. In North America, it affects about 2.5 people per 100,000 each year. About 20-40% of those with IgA nephropathy will develop kidney failure over 20 years. It often shows up after a cold or sore throat, with bloody urine appearing within hours. Post-streptococcal glomerulonephritis is more common in kids. After a strep throat or skin infection, the immune system can misfire and attack the kidneys. The good news? 95% of children recover fully within 6 to 8 weeks. Adults aren’t as lucky - their recovery rates are lower. Lupus nephritis affects half to two-thirds of people with systemic lupus erythematosus. It’s not just a kidney problem - it’s a sign the whole immune system is out of control. With modern treatment, 70-80% of patients avoid kidney failure within 10 years. But without treatment, the risk of dialysis skyrockets.
Why Diagnosis Takes Time - and a Biopsy
There’s no blood test that can tell you exactly what type of glomerulonephritis you have. That’s why a kidney biopsy is the gold standard. A needle is inserted through the back to take a tiny sample of kidney tissue. It’s not risk-free - about 3-5% of patients have bleeding or severe pain afterward. But it’s the only way to see the pattern of damage under the microscope. Interpreting that biopsy? That’s where things get hard. Nephropathologists need 5 to 7 years of specialized training to tell the difference between C3G, IC-MPGN, IgA nephropathy, and other subtypes. Many patients see three or more doctors before getting a clear diagnosis. On average, it takes 4.2 months from when symptoms start to when a biopsy confirms GN. Patients on forums like Inspire.com and Reddit often say the delay is the hardest part. “I thought it was just dehydration,” one wrote. “By the time they told me it was my kidneys, I was already swollen and couldn’t walk up the stairs.”Treatment: Steroids, Side Effects, and New Hope
For decades, corticosteroids like prednisone were the only weapon. They work - about 60-80% of patients see improvement in proteinuria or blood pressure. But the cost is high. Three out of four patients gain weight. One in three gets infections. Nearly one in four develops osteoporosis. One Reddit user shared: “Prednisone gave me two broken spine bones in 18 months. I was 32.” New treatments are changing the game. For C3G, the drug iptacopan - approved by the FDA in early 2023 under breakthrough therapy status - cuts proteinuria by over 50% in 12 months. It targets a specific part of the complement system, leaving the rest of the immune system alone. Another option, eculizumab, blocks a different complement protein. It works well in some patients - but costs about $500,000 a year. That’s why KDIGO guidelines recommend trying standard therapy for at least six months before jumping to these expensive drugs. The future is personalization. Researchers are now using genetic and protein markers to predict who will respond to which treatment. One study showed that combining molecular data with biopsy results improved treatment prediction accuracy from 65% to 85%. Within five years, doctors may be choosing therapies based on your unique immune profile - not just what the biopsy looks like.
What Patients Are Really Living With
Beyond the lab results and drug names, glomerulonephritis changes daily life. Swelling makes clothes tight. Fatigue means skipping work or school. Medication side effects can be worse than the disease itself. On GN support forums, 78% of posts mention edema. 63% worry about steroid side effects. 51% live in fear of kidney failure. But there are stories of hope. One patient on Reddit said: “Started rituximab within two months of diagnosis. Didn’t need dialysis.” Rituximab, a drug that clears out certain immune cells, is now being used off-label for severe IgA nephropathy and IC-MPGN with promising results. The key? Early action. The sooner you catch it, the better your chances. If you’ve had blood in your urine after a cold, unexplained swelling, or persistent high blood pressure, ask your doctor about a urine test for protein and a blood test for creatinine. Don’t wait for symptoms to get worse.The Bigger Picture: Who Gets GN and Why
Glomerulonephritis isn’t evenly distributed. IgA nephropathy is twice as common in East Asia as in North America. Lupus nephritis hits women more than men - especially those of African, Asian, or Hispanic descent. C3G is rare - only 1 to 2 people per million get it each year in Europe - but it’s more common in families with certain genetic mutations. The global market for GN treatments is growing fast. It was worth $2.3 billion in 2022 and could hit $4.7 billion by 2028. That’s because autoimmune diseases are rising, and we’re getting better at diagnosing them. But here’s the dark side: in low-income countries, patients have 70% less access to biopsies and 90% less access to new drugs. A breakthrough therapy in the U.S. might be out of reach for someone in India or Nigeria. Glomerulonephritis is more than a kidney disease. It’s an immune system gone wrong. It’s a biopsy that takes months to schedule. It’s a drug that costs more than a car. It’s fatigue that no one sees. But it’s also a field moving fast - from broad, toxic treatments to precise, targeted ones. And for those caught in the middle, the message is clear: don’t ignore the signs. Your kidneys are fighting a silent war. You can help them win.Can glomerulonephritis be cured?
Some forms of glomerulonephritis can be cured, especially in children with post-streptococcal GN - about 95% recover fully. In adults, complete cure is less common. For IgA nephropathy or C3G, the goal is to stop progression and protect kidney function. With early treatment, many people avoid dialysis for decades. But if scarring sets in, the damage is permanent. Treatment doesn’t always reverse damage - it prevents more.
Is glomerulonephritis hereditary?
Most cases aren’t inherited. But certain types, like Alport syndrome or some forms of C3 glomerulonephritis, have strong genetic links. If multiple family members have kidney disease or hearing loss, genetic testing may be recommended. For the majority of patients, though, it’s an autoimmune trigger - not a gene - that starts the problem.
Can diet help with glomerulonephritis?
Yes, but not as a cure. A low-sodium diet helps control blood pressure and reduce swelling. Limiting protein intake may ease the kidneys’ workload in advanced cases. Avoiding processed foods and added sugars can help manage inflammation. But diet alone won’t stop the immune attack. It’s a support tool - not a replacement for medical treatment.
How do I know if I have protein in my urine?
You can’t see or feel it. The only way to know is through a urine test. A dipstick test at your doctor’s office can detect protein. For accuracy, a 24-hour urine collection or a urine albumin-to-creatinine ratio (UACR) is used. If your UACR is above 30 mg/g, that’s a sign of kidney damage. Many people with GN have levels over 3,500 mg/g.
What’s the difference between nephrotic and nephritic syndrome?
Nephrotic syndrome means you’re losing a lot of protein - more than 3.5 grams a day - leading to swelling, low blood protein, and high cholesterol. Nephritic syndrome means you’re losing red blood cells - causing bloody urine - along with high blood pressure and reduced kidney function. You can have both at the same time. The key difference is protein loss vs. blood loss in the urine.
Can I still exercise with glomerulonephritis?
Yes - if you’re stable. Light to moderate exercise like walking, swimming, or cycling can help with fatigue and blood pressure. But avoid heavy lifting or contact sports if you’re on immunosuppressants or have high blood pressure. Always check with your nephrologist first. Exercise won’t fix your kidneys, but it can help you feel better while you’re treating them.
How often do I need blood tests?
When you’re first diagnosed or starting treatment, expect blood tests every two weeks to check creatinine and electrolytes. Once stable, monthly checks are typical. Urine protein tests should be done monthly too. If you’re on a new drug like iptacopan or rituximab, your doctor may monitor you more closely - sometimes every two weeks for the first few months.


Comments
Annie Choi
January 17, 2026 AT 03:33Just got diagnosed with IgA nephropathy last month and honestly this post nailed it. Fatigue is real. Swelling feels like I'm wearing water wings 24/7. Started on prednisone and already my face looks like a balloon. But I'm trying to stay positive. Found a local support group and we swap tips on low-sodium snacks. You're not alone.
Dan Mack
January 17, 2026 AT 21:12They say it's autoimmune but who really controls the immune system? Big Pharma. They want you dependent on $500k drugs so you keep coming back. Biopsies? That's how they lock you into the system. The real cure is detoxing your liver and avoiding fluoride in the water. They don't tell you that.
Amy Vickberg
January 18, 2026 AT 13:50Thank you for writing this with so much clarity. I'm a nurse and I see patients with GN all the time. The delay in diagnosis breaks my heart. One woman waited 8 months because her doctor kept saying it was just stress. By then she was at 30% kidney function. Early testing saves lives. Please get that UACR test if you're even slightly concerned.
Nat Young
January 20, 2026 AT 13:14Let's be real. The entire field of nephrology is built on guesswork. Biopsies are invasive, expensive, and often inconclusive. They call it 'C3G' like it's a brand name. Meanwhile, 70% of patients respond to nothing. And now they're pushing iptacopan like it's magic? It's just another drug that shifts the problem downstream. We're treating symptoms, not causes. And the real cause? Environmental toxins, glyphosate, microplastics. No one wants to say it because it's not profitable.
Niki Van den Bossche
January 20, 2026 AT 14:42It's not just a disease-it's a metaphysical rupture. The glomeruli are the soul's filtration system. When the immune system turns on them, it's the body screaming that the soul has been betrayed. Modern medicine sees proteins and antibodies. I see a cry for alignment. The body doesn't attack itself unless it's been spiritually violated. Have you asked yourself what you're refusing to feel? The kidneys hold grief. Your proteinuria? It's your tears leaking out.
Jan Hess
January 20, 2026 AT 19:43Biggest mistake people make? Thinking steroids are the endgame. I was on prednisone for 18 months. Gained 50 pounds, broke two vertebrae, got shingles twice. Then I found rituximab. Changed everything. No more swelling. No more crushing fatigue. My creatinine dropped from 2.1 to 1.0 in 4 months. If you're still on steroids and not improving-ask your doc about B-cell depletion. It's not experimental anymore. It's life-changing.
Iona Jane
January 22, 2026 AT 06:19They're hiding the truth. The CDC knows that 80% of GN cases are linked to mRNA vaccines. Look at the spike in cases after 2021. Why are they calling it 'autoimmune'? Because they don't want to admit they poisoned us. My cousin died waiting for a biopsy. They said it was 'idiopathic'. I say it was injected. Don't trust the system. Fight for your life.
Jaspreet Kaur Chana
January 24, 2026 AT 05:35Here in India, we don't even have access to basic urine tests in rural areas. My uncle had GN and they thought it was just water retention. He was 42. Died before they even did a biopsy. We need awareness. Not just in the US or Europe. In villages where people walk 10km to a clinic. A simple dipstick test could save thousands. Why is no one talking about this? The global market is growing but the people are dying in silence. We need mobile health units. We need low-cost diagnostics. This isn't just science-it's justice.
Haley Graves
January 26, 2026 AT 05:06Don't let the fear paralyze you. I was told I'd be on dialysis by 40. Now I'm 47. Still working. Still hiking. I take iptacopan. I track my UACR like a pro. I eat clean. I sleep 8 hours. I don't stress. You can't control the disease-but you can control your response. Your kidneys are warriors. So are you. Keep showing up.
Diane Hendriks
January 26, 2026 AT 14:17There is a critical grammatical error in the original post. The phrase '3 to 5 times higher than normal' is statistically imprecise. It should read 'three- to fivefold increase' or '300% to 500% elevation'. This matters because in nephrology, precision in language reflects precision in science. Sloppy phrasing undermines credibility. Also, 'nephrotic syndrome' is not defined correctly-it's not merely 'protein loss' but specifically >3.5 g/day with hypoalbuminemia, edema, and hyperlipidemia. Fix your terminology before you lecture the public.
ellen adamina
January 28, 2026 AT 12:23My mom had this. She didn't even know she was sick until her legs swelled up like balloons. She was 58. Biopsy took 3 months. They told her it was IgA. She didn't get the new drugs. Just steroids. She lost her job. Lost her hair. Lost her energy. But she never complained. She just kept making tea. I wish someone had told her about rituximab earlier. If you're reading this and you have blood in your urine after a cold-don't wait. Get tested. Please.