Diagnosing Chronic Idiopathic Constipation: Key Signs, Methods, and Practical Insights
Bloating so bad your jeans refuse to zip up and endless bathroom struggles with no relief—chronic idiopathic constipation (CIC) isn’t just embarrassing. It can take over your whole day. You try to eat more fiber. You swap your morning coffee for green smoothies. Still, nothing budges, and you’re beginning to wonder: Why doesn’t anything work? And what if you’re chasing the wrong problem altogether? The reality is, diagnosing CIC is trickier than most people think. It hides behind symptoms that keep you guessing and frustrate even some doctors. Decoding this stubborn gut problem takes careful detective work, a real understanding of the gut, and, honestly, some patience you probably don’t have right now. Let’s break down what it really takes to figure out if stubborn constipation is actually CIC—and not caused by something else you haven’t even heard of yet.
Unpacking Chronic Idiopathic Constipation: Symptoms, Red Flags, and Distinguishing It from Other Conditions
You’d think constipation would be all about how many times you don’t go, but there’s way more to it. People with CIC can just as easily be dealing with abdominal pain, a weird sense of fullness, or stools so hard they leave you dreading every trip to the bathroom. Officially, CIC means you’ve had slow, hard, or incomplete stools—at least three months, and at least two symptoms like straining, lumpy stools, or a feeling that you just can’t finish. It’s not just missing a day or two here and there.
The tricky thing is, CIC gets called 'idiopathic' because doctors haven’t nailed down a medical explanation, even after tests. There’s no obvious cause—no medication, no obvious gut disease, no structural issue. Stats actually show that as many as 16% of adults have constipation, but only 1 in 10 gets officially diagnosed with chronic idiopathic constipation, because the rules are strict and so many things can mimic its symptoms. If you’re wondering, women seem to get hit about twice as often as men, especially after age 50, though doctors aren’t sure exactly why.
One of the hardest parts is sorting CIC from other constipation types, like irritable bowel syndrome with constipation (IBS-C), medication-induced slowdowns, or thyroid problems. IBS-C, for example, involves constipation with episodes of pain that disappear after going to the bathroom—IBS-C is also more likely to come with gas or diarrhea swings. Some red flags should push doctors to look for something more serious: blood in the stool, sudden weight loss, waking up at night with pain, or a family history of colon cancer. These aren’t CIC and should always get fast attention.
- Key symptoms for CIC diagnosis:
- Fewer than three bowel movements per week
- Straining with more than 25% of defecations
- Stools that are hard or lumpy for more than 25% of bowel movements
- Sensation of incomplete evacuation or blockage
- Reliance on manual maneuvers to help stool pass
You’d be amazed how much habits matter, too. People who ignore the urge to go or who have lots of lifestyle changes (think travel, night shifts) often find symptoms come and go, confusing the diagnosis. Kids and older adults get mismarked all the time, since constipation means different things at different ages.
The Rome IV criteria (think of it as the official checklist) sets the gold standard here—doctors use it to pick apart different patterns and rule out temporary issues. One forgotten fact: most people with CIC don’t report symptoms right away, meaning that by the time you show up to the doctor, the problem might have been brewing for months or years. That’s why doctors always want a full symptom diary—more on that soon.
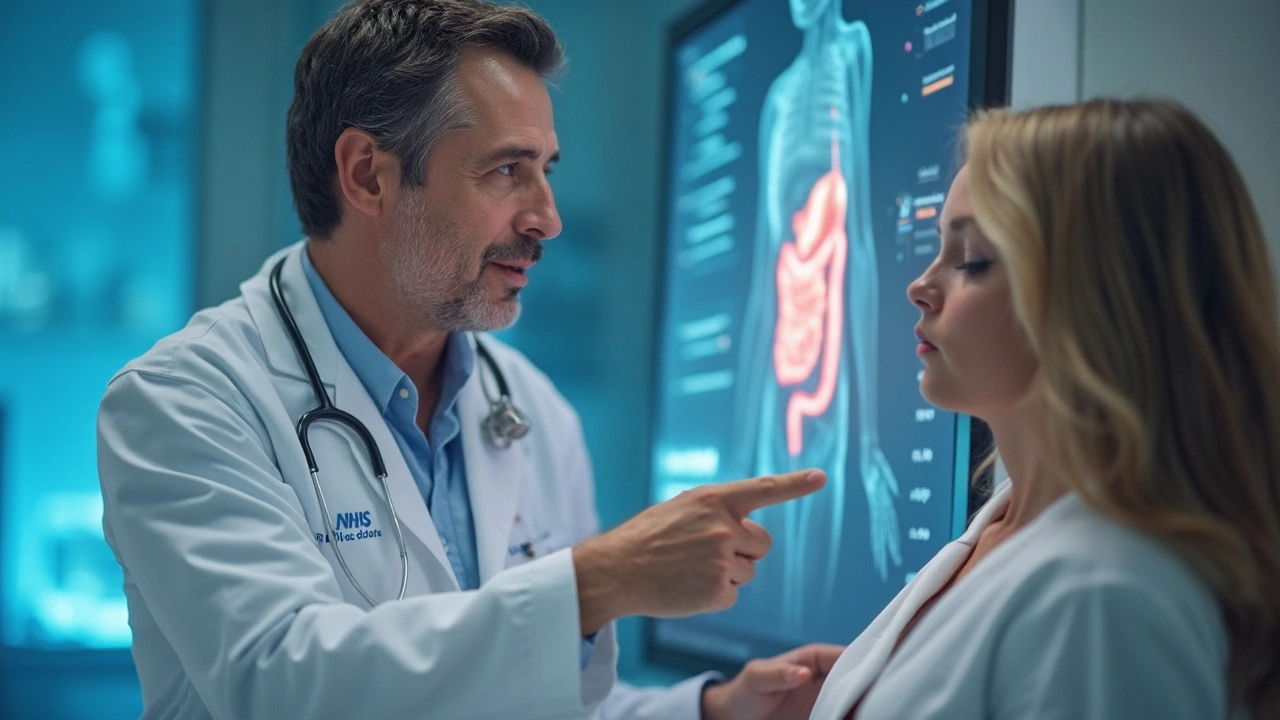
Diagnostic Workup: What Doctors Look For and How Testing Unfolds
So you’ve got stubborn constipation, nothing is working, and your doctor suspects CIC. Now what? It starts, honestly, with questions. Lots of questions. The most useful tool, surprisingly, is still a simple discussion: How long has this been happening? Any sudden changes? What’s your diet like? Key info includes details about stool frequency, consistency (a Bristol Stool Chart can help), use of laxatives or fiber, meds, sleep, stress, even periods for women. Keep a diary for two weeks—it’s more valuable than you think.
Doctors usually start with bloodwork to double-check it’s not something obvious, like low thyroid (hypothyroidism), high calcium, or diabetes. Sometimes, they'll run a complete blood count (CBC), check for celiac disease markers, and measure electrolytes. These rule out sneaky medical triggers that love to wear constipation as a disguise. If nothing pops up, and there are no red-flag symptoms (remember the warning signs—weight loss, blood in stool, family history of colon cancer), then CIC becomes the working diagnosis.
Physical exams are surprisingly revealing. Docs usually check your belly for tenderness, masses, or weird sounds, and sometimes do a rectal exam to spot fissures, hemorrhoids, or impaction. Don’t love the idea? Totally normal—but honestly, it’s one of the fastest ways to rule out a pile-up or blockage that would change everything about your treatment plan.
At this point, the Rome IV criteria steps in again. Think of it like a referee, making sure nobody’s cutting corners. If you’ve had symptoms for at least six months, and nothing else explains your constipation, you likely meet the criteria for CIC. Kids and older adults get special checklists, given how different things can look for them.
Still, not everyone fits perfectly into a checklist. If symptoms look weird or don’t respond to classic treatments, doctors start reaching for more advanced tools. You might hear about colon transit studies (x-rays after swallowing a marker pill), anorectal manometry (measuring pressure in your rectum), or balloon expulsion tests (no, not as crazy as they sound). Here’s a quick breakdown of these advanced tests, with a sample data table so you can see what they'd look for:
| Test | Purpose | Sample Data Point | Typical Finding in CIC |
|---|---|---|---|
| Colonic Transit Study | Measures time for markers to pass through colon | Time > 72 hours | Delayed transit in slow-transit CIC |
| Anorectal Manometry | Assesses anal and rectal muscle function | Abnormal sphincter relaxation patterns | Normal or minor abnormalities |
| Balloon Expulsion Test | Test ability to expel a small balloon from rectum | Time to expel > 1 minute | Possible outlet obstruction |
| Blood Tests | Rules out metabolic causes | Normal TSH, calcium, glucose | Normal in CIC |
Most of these tests are reserved for tough cases—if you respond to changes in fiber, fluid, or over-the-counter remedies, you may never need to see them. But if your gut just won’t budge, these become the gold standard for finding hidden causes.
Rather weirdly, colonoscopies aren’t routine for CIC unless you’re over 50 or have warning signs. The reason? Most people under 50 with just constipation and no red flags have a low risk of hidden serious disease, and colonoscopies carry their own risks and discomforts.
Tips for Getting an Accurate Diagnosis and When to Seek Extra Help
Getting an accurate CIC diagnosis isn’t about going it alone. Think of yourself as the main investigator, with your doctor acting as the consultant who helps sort out which clues matter. Start by keeping a detailed symptom diary—not just "I haven’t gone for three days," but tracking exactly how often, stool type (be honest), any pain, foods eaten, medications, and things like stress or travel. If you notice a pattern (for instance, things get worse after dairy or during stressful weeks), mention it. Use smartphone apps made for gut tracking or just jot things in a notebook—either way, you’ll end up with clues most doctors love to see.
Be totally honest about laxative use. Some people underreport or skip this because it feels embarrassing, but doctors see it all the time—truth makes for a faster, more accurate diagnosis. Certain lifestyle habits like holding it in (common among nurses and teachers), not drinking enough fluids, or keeping an erratic sleep schedule can all muddy the waters, so lay it out openly.
If you’ve already tried upping your fiber and fluids (and given it at least 3-4 weeks to work), let your healthcare provider know. Sometimes, overdoing fiber or using the wrong kind (insoluble versus soluble) can actually make things worse, causing more bloating or cramping. Soluble fiber (like the kind in oats, apples, or psyllium husk) is often gentler than insoluble fiber (found in bran or raw veggies). Strategies like regular exercise and setting aside consistent 'toilet time' every day (ideally 20 minutes after breakfast for most people) can trigger natural gut movement. None of these are guaranteed, but they make a real difference for a portion of people stuck in a constipation rut.
Don’t be surprised if your doc wants to check on your mental health, too. Depression, anxiety, and even simple stress are connected to gut slowdowns, thanks to the gut-brain axis. If you’re noticing mood shifts alongside constipation, flag it—it could be the missing piece.
- chronic idiopathic constipation gets confused with IBS, medication side effects, and hormonal issues
- Symptom diaries (written or digital) provide the best trail for diagnosis
- Look for symptoms that aren’t explained by food, stress, or travel—if anything feels sudden or severe, seek attention fast
- Don’t self-treat with high doses of laxatives for more than 2-3 weeks without checking in with a care provider
- Ask about genetic and family health patterns if you haven’t already
The truth is, diagnosing CIC isn’t always fast or simple, but it can be done correctly with a solid partnership between you and your doc. Don’t settle for quick fixes—push for answers if something feels off, especially with weird or persistent symptoms. The sooner you nail down the cause, the faster your gut (and your jeans) can get back to normal.


Comments
Mohamed Aseem
May 19, 2025 AT 08:47Bro this is just another medical textbook repackaged as a Reddit post. I’ve had this for 12 years and no doctor ever gave me a damn clue-just ‘eat more fiber’ like I’m a damn rabbit. Meanwhile my colon’s out here on strike and your ‘Rome IV criteria’ won’t even let me pee in peace. You think I care about stool consistency charts when I’m crying in the bathroom at 3 AM? This isn’t science-it’s a fucking checklist for doctors to feel smart while I suffer.
Steve Dugas
May 19, 2025 AT 17:00Incorrect. The Rome IV criteria are not a checklist-they’re a diagnostic framework grounded in longitudinal symptom analysis. You’re conflating symptom management with diagnostic validity. Fiber intake is not a panacea, but its efficacy is modulated by soluble versus insoluble composition, which you clearly ignore. Furthermore, the absence of red flags negates the need for colonoscopy in under-50s per ACG guidelines. Your emotional outburst doesn’t invalidate clinical methodology-it reveals a fundamental misunderstanding of evidence-based medicine.
Paul Avratin
May 20, 2025 AT 15:28There’s something deeply poetic about the way our modern bodies rebel against the rhythm of industrialized life. The colon-once a sacred vessel of slow digestion, of ancestral patience-is now a battleground against processed food, digital distraction, and the tyranny of productivity. CIC isn’t just a medical condition-it’s a silent scream from the autonomic nervous system, begging us to slow down. The Bristol Chart? It’s not just about stool shape. It’s about the soul’s rhythm. When your body won’t move, maybe your spirit hasn’t either.
Brandi Busse
May 21, 2025 AT 16:30Ugh I hate when people act like constipation is some deep mystery like it’s a damn yoga pose. I tried everything fiber psyllium probiotics even that weird apple cider vinegar thing. Nothing worked until I stopped holding it in at work because I was too busy scrolling. Like duh. Also why is everyone so obsessed with tests. I just wanted a pill that didn’t make me cramp like I was giving birth. Also I’m pretty sure my cat has better bowel habits than me
Colter Hettich
May 22, 2025 AT 13:08One cannot help but observe, with a certain existential melancholy, the way contemporary medicine reduces the ineffable complexity of human physiology to algorithmic checklists-Rome IV, Bristol Chart, transit times-as if the body were a machine to be calibrated, rather than a living, breathing paradox of biochemistry and psyche. The ‘idiopathic’ in CIC is not a failure of diagnosis, but an admission of our profound ignorance: we measure, we classify, we label… yet we do not comprehend. The colon remembers trauma. It holds grief. It resists not because of diet, but because the self has forgotten how to yield.
Prem Mukundan
May 23, 2025 AT 17:27Listen I’ve seen this in my clinic for 15 years. People think it’s just ‘not pooping’ but it’s usually lifestyle wrapped in denial. You’re sitting 10 hours a day drinking soda, ignoring the urge because you’re ‘too busy’, then blaming the gut. And don’t even get me started on laxative abuse-people think it’s harmless until their colon turns into a lazy slug. Fix your schedule, drink water, move. No test needed. If it’s still bad after 30 days? Then yeah, see a doc. But 90% of this is just bad habits dressed up as a medical mystery.
Leilani Johnston
May 25, 2025 AT 00:03Hey I just wanna say you’re not alone. I had this for years and felt so ashamed until I started journaling my days-not just poop, but stress levels, what I ate, how I slept. Turns out my anxiety spiked every time I worked late and my gut just… shut down. I started doing 5 minutes of breathing before bed and walking after dinner. It’s not magic, but it helped. And it’s okay to need meds sometimes-no shame. Your body’s trying to tell you something. Listen to it. You got this.