Celiac Disease: How to Live Gluten-Free and Fix Nutrient Deficiencies

Living with celiac disease isn’t just about avoiding bread or pasta. It’s about rebuilding your body from the inside out. When you eat gluten, your immune system attacks your small intestine. Over time, this damages the villi - tiny finger-like projections that absorb nutrients. Without them, your body can’t get the vitamins and minerals it needs, no matter how much you eat. The result? Fatigue, anemia, bone loss, brain fog, and more. But here’s the good news: if you cut out gluten completely and fix the nutrient gaps, most symptoms disappear within weeks. The problem? Most people don’t know how to do it right.
What Exactly Is Gluten-Free Living?
Gluten is a protein found in wheat, barley, rye, and their close relatives like spelt and triticale. For someone with celiac disease, even a tiny crumb - like 50 milligrams - can trigger damage. That’s about the size of a crouton. So, gluten-free isn’t just swapping bread brands. It’s a total lifestyle shift. Safe foods include rice, quinoa, buckwheat, corn, potatoes, and certified gluten-free oats. But here’s where people get tripped up: gluten hides everywhere. Soy sauce, malt vinegar, processed meats, salad dressings, and even some medications contain gluten. And cross-contamination? It’s everywhere. A toaster used for regular bread, a shared cutting board, or a fryer that’s cooked chicken nuggets and fries? Those are all minefields. A 2024 study found that 85% of people with celiac disease who still feel unwell are unknowingly exposed to gluten. Most of it comes from restaurants or shared kitchens. That’s why many people need separate utensils, a dedicated toaster, and even separate condiment jars. Reading labels isn’t enough anymore. You need to understand what’s behind the words. "Wheat-free" doesn’t mean gluten-free. "Natural flavors" could contain barley. Always look for the certified gluten-free seal - it means the product has been tested to contain less than 20 parts per million of gluten.Why Nutrient Deficiencies Are So Common
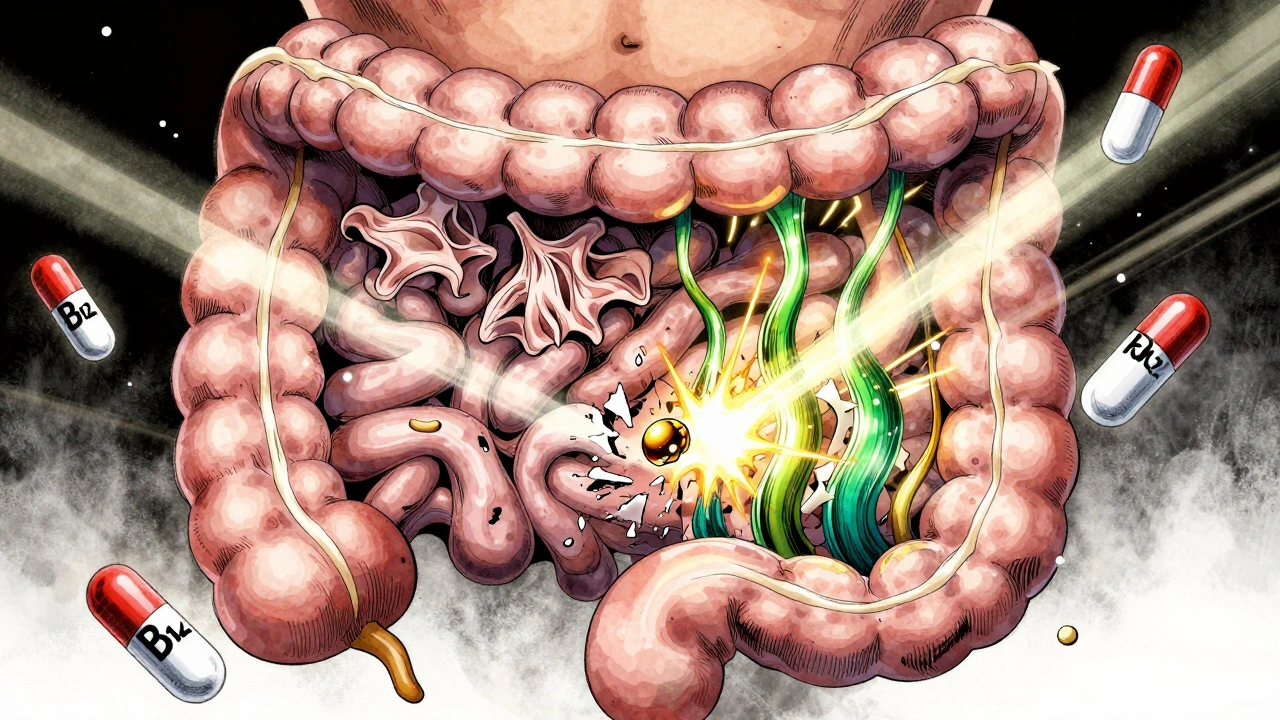
When your small intestine is damaged, it can’t absorb nutrients properly. That’s why nearly every newly diagnosed person has at least one major deficiency. Iron deficiency anemia affects 12% to 63% of patients. Vitamin D deficiency hits 37% to 75%. Calcium is low in 25% to 40%. B vitamins, especially folate and B12, are often depleted too. These aren’t random gaps. They’re direct results of intestinal damage. Iron absorption happens in the duodenum - the first part of the small intestine - which is usually the most damaged in celiac disease. That’s why so many women with celiac feel exhausted, dizzy, or short of breath. Vitamin D and calcium are absorbed further down, but if the whole lining is thinning, both suffer. Bone density drops fast. A DXA scan (a type of bone scan) often shows osteopenia or osteoporosis at diagnosis. Even after going gluten-free, deficiencies don’t always fix themselves. Healing takes time - sometimes up to two years. And if your diet is still full of processed gluten-free junk food (which is often low in fiber, iron, and B vitamins), you’ll stay deficient. That’s why supplements aren’t optional. They’re part of your recovery plan.What to Supplement - and How Much
Here’s what most people with celiac need, based on clinical guidelines from 2025:- Iron: 18 mg daily for women, 8 mg for men. If you’re anemic, your doctor may prescribe higher doses or even IV iron. Oral iron can cause stomach upset - take it with vitamin C to help absorption.
- Vitamin D: 600-800 IU daily is the minimum. Most people need 1,000-2,000 IU, especially in winter. Some need 5,000 IU short-term to correct severe deficiency. Get your blood levels checked.
- Calcium: 1,000-1,200 mg daily. Don’t rely on dairy if you’re also lactose intolerant (common with celiac). Use fortified plant milks or calcium citrate supplements.
- Folate (B9): 400 mcg daily. Look for methylfolate, not folic acid - some people with celiac can’t convert folic acid properly.
- Vitamin B12: 250-500 mcg daily. Sublingual (under-the-tongue) forms work better if your gut is still healing. Some need 1,000 mcg if levels are very low.
- Magnesium: 400 mg daily. Helps with muscle cramps, sleep, and nerve function. Many gluten-free diets are low in magnesium-rich foods like nuts and leafy greens.
Don’t just buy any supplement. Look for brands labeled "gluten-free" and certified by third parties like NSF or GFCO. Some cheap supplements use gluten-containing fillers like wheat starch. Always check the label.
Diagnosis and Monitoring: What You Need to Know
You can’t self-diagnose celiac. If you suspect you have it, get tested before going gluten-free. The test - tissue transglutaminase IgA (tTG-IgA) - is 98% accurate if you’re still eating gluten. But 2-3% of people have IgA deficiency, so total IgA levels must be checked too. If the blood test is positive, an endoscopy with biopsy is usually needed to confirm. New guidelines from 2025 allow some children to be diagnosed without a biopsy if they have very high antibody levels, symptoms, and genetic markers. For adults, biopsy is still standard - unless your doctor uses a newer test called epithelial lymphogram, which has 98% specificity and is now being used in Europe. After diagnosis, follow-up is critical. At three months, you should have a blood test for tTG-IgA to see if levels are dropping. At six months, check nutrient levels again. A bone density scan is recommended every two to three years. If symptoms persist after a year on a gluten-free diet, you may have non-responsive celiac disease - meaning your gut isn’t healing. That’s when you need deeper testing: capsule endoscopy, microbiome analysis, or even a repeat biopsy.The Hidden Challenges of Going Gluten-Free
The biggest myth? That gluten-free is easy now. Yes, there are more products than ever. But they’re expensive. Gluten-free bread costs nearly 160% more than regular bread. A box of gluten-free pasta can be $5 instead of $1.50. That’s a huge burden. Dining out is still risky. Only 28% of U.S. restaurants have verified gluten-free protocols. Even if the chef says "we don’t use gluten," cross-contamination is common. Use a restaurant card - the Celiac Disease Foundation offers them in 30+ languages - to explain your needs clearly. Medications are another blind spot. About 30% of prescription pills contain gluten as a filler. The University of Chicago maintains a free Gluten-Free Drug Database. Always ask your pharmacist to check. And then there’s the emotional toll. Social isolation, constant vigilance, and feeling like a burden can lead to anxiety or depression. Support groups - online or in-person - make a huge difference. Reddit’s r/celiac has over 100,000 members sharing tips, recipes, and real stories.
What Works: Real Stories, Real Results
One patient in Melbourne, Australia, struggled with chronic fatigue for years. Her blood tests showed low iron and B12. She went gluten-free but still felt awful. After meeting with a dietitian who specialized in celiac, she started taking methylfolate and sublingual B12. Within six weeks, her energy returned. Her tTG-IgA levels dropped to normal within four months. Another family in Texas had a 7-year-old with failure to thrive. He wasn’t gaining weight. His doctor diagnosed celiac, but the family didn’t know how to feed him properly. They started with a nutritionist who created a simple meal plan: eggs, rice, chicken, bananas, and certified gluten-free oats. Within three months, he gained 8 pounds. His bone density improved over the next year. The pattern? Success doesn’t come from just avoiding gluten. It comes from replacing what was lost - with the right nutrients, the right foods, and the right support.What’s Next for Celiac Disease?
Scientists are working on alternatives to the gluten-free diet. Enzyme therapies like Latiglutenase are in Phase 3 trials - they break down gluten in the stomach before it reaches the intestine. A vaccine called Nexvax2 showed promise but didn’t work in Phase 2. Gluten-detecting devices like the Nima Sensor let you test your food in seconds - they’re 90% accurate at detecting gluten above 20 ppm. But right now, the only proven treatment is still a strict gluten-free diet. And the only way to heal your body fully is to pair that diet with targeted nutrient support. No shortcuts. No magic pills. Just consistency. If you’ve been diagnosed, don’t wait to fix your deficiencies. Get your blood tested. Talk to a dietitian who knows celiac inside and out. Don’t assume your doctor will tell you everything - most don’t get training in nutritional rehab. Take charge. Your gut will thank you. Your bones will thank you. And your energy? It’ll come back.Can I eat oats if I have celiac disease?
Most people with celiac disease can safely eat certified gluten-free oats - but only if they’re labeled as such. Regular oats are almost always contaminated with wheat or barley during farming or processing. Start with small amounts (50g per day) and monitor for symptoms. About 5% of people still react, so stop if you feel bloated, tired, or get diarrhea. Always choose oats certified by GFCO or similar.
Why do I still feel tired after going gluten-free?
Fatigue often means you’re still deficient. Iron, B12, vitamin D, and magnesium are the most common culprits. Even if you’re avoiding gluten, your diet might still lack nutrient-dense whole foods. Processed gluten-free snacks don’t fix deficiencies. Get blood work done and consider supplements under a doctor’s guidance. Healing takes time - up to two years for full intestinal recovery.
Is a gluten-free diet healthy if I don’t have celiac disease?
Not necessarily. Many gluten-free products are lower in fiber, iron, and B vitamins because they’re made with refined starches instead of whole grains. Unless you have celiac disease, non-celiac gluten sensitivity, or a doctor-recommended reason, cutting out gluten offers no proven health benefit - and may lead to nutrient gaps. Whole wheat bread is often healthier than gluten-free white bread.
How do I know if my supplements are gluten-free?
Look for certification labels like GFCO (Gluten-Free Certification Organization) or NSF Certified for Gluten-Free. Avoid products with vague terms like "manufactured in a facility that also processes wheat." Call the manufacturer if you’re unsure. Some brands list all ingredients - including fillers - on their website. When in doubt, choose a brand trusted by the celiac community.
Can celiac disease be cured?
No, there is no cure yet. The only treatment is lifelong, strict avoidance of gluten. But with proper diet and nutrition, the intestinal damage heals, symptoms disappear, and long-term risks - like cancer and osteoporosis - drop to near-normal levels. Many people live completely normal, healthy lives once they get the right support.


Comments
Aileen Ferris
December 11, 2025 AT 01:03gluten free is just a trend anyway lol who even cares bout villi
Neelam Kumari
December 11, 2025 AT 14:03So you're telling me I need to spend $20 on a loaf of bread and take 6 supplements just to not feel like a zombie? Wow. I guess my $3 sourdough wasn't good enough.
Doris Lee
December 12, 2025 AT 05:32This is the most helpful post I've read all year. Seriously. I was so lost after my diagnosis. Thank you.
Regan Mears
December 13, 2025 AT 06:45I was skeptical at first, but after 18 months of strict GF + B12 + magnesium, my brain fog lifted and my energy is back. It's not magic-it's medicine. You've got this.
Michaux Hyatt
December 15, 2025 AT 02:04Don't forget about zinc! A lot of people with celiac are deficient and it affects immune function and taste. I started taking 15mg daily and my appetite came back. Also, try quinoa flakes for breakfast-they're a game changer.
Michelle Edwards
December 15, 2025 AT 14:49I used to think gluten-free was just about bread. Then I realized my salad dressing had malt vinegar. And my multivitamin had wheat starch. And my toothpaste? Yeah. It's exhausting. But worth it.
Nikki Smellie
December 17, 2025 AT 01:57I've been reading about this for years... and I'm starting to think the whole celiac industry is a pharmaceutical scam. What if gluten isn't the problem? What if it's glyphosate? Or the gut microbiome? Or the fact that we're all just too stressed? The FDA is hiding something. I've seen the documents.
Sarah Clifford
December 18, 2025 AT 06:23I went gluten-free and now I'm depressed because my friends won't eat with me and my mom thinks I'm doing it for attention. I just want to eat pizza without feeling like I'm dying. Why is this so hard?
Regan Mears
December 19, 2025 AT 23:14It's not about attention. It's about survival. I used to cry in the grocery store because nothing was safe. But now I have my own toaster, my own soy sauce, and my own peace. It's not easy-but you're not alone.
Frank Nouwens
December 20, 2025 AT 00:31The assertion that nutrient deficiencies are a direct consequence of villous atrophy is well-supported by longitudinal studies, particularly those conducted by the University of Chicago Celiac Disease Center. Furthermore, the recommended supplementation protocols align with the 2025 International Celiac Society Guidelines. One might argue that the dietary burden is substantial, yet the alternative-continued mucosal injury-is far more deleterious.
Ben Greening
December 21, 2025 AT 12:43I appreciate the thoroughness of this post. As someone who's been gluten-free for 12 years, I can confirm: the certified seal matters. I once took a cheap supplement labeled 'gluten-free' and ended up with a flare-up. Turned out it had barley malt extract. Always check the certification. It's not paranoia-it's protocol.
Queenie Chan
December 22, 2025 AT 06:33I used to think gluten was the villain... until I started eating sprouted ancient grains and noticed my bloating vanished. Now I wonder-what if it’s not the gluten, but the modern processing? The way wheat is hybridized? The pesticides? The way we bake it? Maybe the real issue isn’t the protein... but the whole damn system. Just saying.
David Palmer
December 22, 2025 AT 14:16I tried going gluten-free and I felt worse. Like, way worse. I think it’s all in my head. Or maybe I’m just allergic to being told what to eat. I’m gonna eat what I want and let the chips fall.